News release
From:
Drug-resistant superbug spreading through hospitals undetected
Melbourne clinician and genomic researchers have uncovered a bacterium persisting in Victorian hospitals and around the world, capable of causing near untreatable infections.
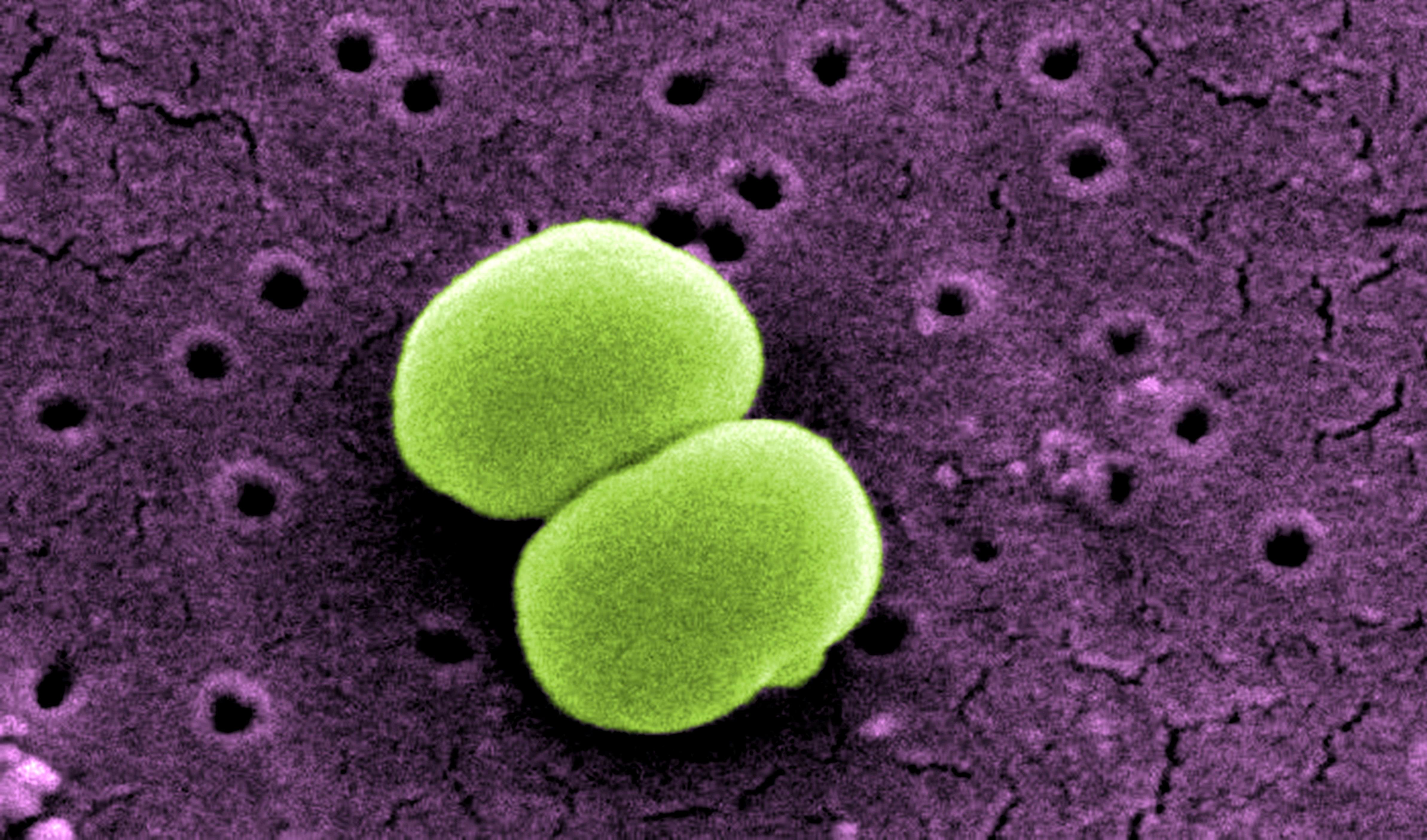
Multidrug-resistant Staphylococcus epidermidis (S. epidermidis) is a leading cause of hospital-acquired infections, but far less is known about this organism than its cousin, methicillin-resistant Staphylococcus aureus (MRSA).
Found on the skin of all humans, S. epidermidis often contaminates diagnostic samples, meaning it is frequently dismissed as a false positive result.
Published today in Nature Microbiology, Peter Doherty Institute for Infection and Immunity (Doherty Institute) researchers looked at hundreds of S. epidermidis isolates from 78 institutions in 10 countries around the world, and found three strain sub-types that have spread globally and are resistant to nearly all antibiotics.
Most alarming was the discovery that some of the strains discovered in Europe are resistant to all known antibiotics.
Study author, University of Melbourne Professor Ben Howden, Director of the Microbiological Diagnostic Unit Public Health Laboratory at the Doherty Institute, said S. epidermidis infects people who are immunocompromised or have had prosthetic materials implanted, such as catheters and joint replacements.
“The discovery of these new strains means we are now routinely using our last-line antibiotics that are expensive and toxic. This makes these S. epidermidis infections very costly and difficult-to-treat,” Professor Howden said.
Doherty Institute PhD student and first-author on the paper, Dr Jean Lee, was able to show that S.epidermidis made a small change in its DNA that led to resistance to two major antibiotics.
“These two antibiotics are unrelated and you would not expect one mutation to cause both antibiotics to fail,” Dr Lee said.
“Our study suggests current guidelines for treating these infections with the combination of these two antibiotics that were thought to protect one another against developing resistance are based on an incorrect assumption, and that current treatment recommendations need to be reviewed.”
The researchers suggest the reason for the spread of these S. epidermidis strains is likely two-fold. Firstly, catheters and other implanted devices are frequently impregnated with antibiotics as a strategy to prevent infection, however this approach is likely promoting the development of resistance.
Secondly, these infections are most prevalent in intensive care, where patients are sickest and strong antibiotics liberally prescribed, promoting the development of additional resistance.
Professor Howden said the extent of the spread of these antibiotic-resistant strains highlight that we need to be a lot more aware of this as a problem in our hospitals, not just here in Victoria, but around the world.
“There is an urgent need for an international monitoring system to understand the prevalence and impact of S. epidermidis and to systematically measure antibiotic resistance and infections due to this pathogen,” he said.
“We need a better understanding of how S. epidermidis is persisting in hospitals, because it’s happening in an era where MRSA is disappearing through good infection control measures,” Professor Howden said.
This project was a collaboration between the Doherty Institute, Austin Health and Monash Health in Australia, and a number of international institutes.
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Associate Professor Sanjaya Senanayake is a specialist in Infectious Diseases and Associate Professor of Medicine at The Australian National University
'Staph infection' usually refers to 'golden Staph' (or Staphylococcus aureus); however, on our skin live lots of other staphylococcal species, known as coagulase-negative staphylococci (CoNS).
Although the CoNS are regarded as less aggressive than golden staph, the CoNS do cause serious infections. These relate to infections of medical devices, where CoNs have the ability to form a thick surface layer called a 'biofilm' that protects them from antibiotics and the immune system.
Examples include infections of joint replacements (knees, hips etc), urinary catheters, artificial heart valves, cardiac devices, central venous catheters (causing septicaemia) and extra-ventricular drains (causing meningitis).
Infections by CoNS in these settings can be life-threatening. The current study discovered that subgroups of one common type of CoNs (Staphylococcus epidermidis) have become resistant to nearly all antibiotics normally available to treat them. This was found here in Australia and elsewhere around the world.
They postulate antibiotic use and possibly use of certain antibiotic-impregnated devices as driving the emergence of this very resistant strain.
Given the increasing prevalence of hospital-acquired infections and the widespread presence of joint replacements, these infections are likely to become more significant in the future.
This is another example of 'antibiotic resistance' which, if unchecked, is predicted to cause tens of millions of deaths/year in 2050 at a cumulative cost of 100 trillion dollars of economic output.
Associate Professor Rietie Venter is the Head of Microbiology at the University of South Australia
A benign component of our microbiota turns in to a multi-drug resistant superbug. This is one of the newest threats on our ongoing struggle with antimicrobial resistance identified in this study.
Staphylococcus epidermidis is an abundant organism found as part of our skin microbiome. Relative proportions of the family Staphylococcaceae are the highest on moist parts of the skin such as the inner elbow and the back of the knee, with S. epidermidis making up a large part of this family. S. epidermidis is mostly a beneficial bacterium that also ensures a healthy skin microbiome by keeping the growth of other more pathogenic strains such as Staphylococcus aureus in check.
However, S. epidermidis is increasingly emerging as a hospital-acquired pathogen that could cause infections associated with implants etc. Device impregnation with antimicrobials is a standard way to limit device associated infections.
Due to the propensity of resistance to develop when only one antibiotic is used a combination of two antibiotics, rifampicin and vancomycin, are clinically used to prevent infections from staphylococci.
However, this study has shown that the global spread of three clones of S. epidermidis with resistance to both rifampicin and vancomycin. Vancomycin (and teicoplanin) are antibiotics used to treat resistant staphylococci such as methicillin resistant Staphylococcus aureus (MRSA), therefore resistance to these last line of drugs is a cause for serious concern.
Even more worryingly, strains of S. epidermidis were also isolated that were additionally resistant to another last resort drug linezolid and to daptomycin (a very effective antibiotic with hardly any previous reports of resistance).
Therefore, the effectiveness of dual therapy to combat device-related infections should be reinvestigated as the outcome of this could be an increase in pan-drug-resistant organisms causing untreatable infections.
Staphylococcus epidermidis is a bacterium commonly found on our skin. The prevalence of this opportunistic bacterium makes it a first suspect in blood infection when the integrity of the skin is compromised.
This study highlights several key findings including widespread resistance emergence in the bacterium, driven by impregnating medical devices with antibiotics.
Alarmingly, the study also reports that S. epidermidis clinical isolates are less sensitive to antibiotics commonly used to treat it and are thus harder to treat. In one case, the authors report the presence of isolates from German hospitals that are resistant to all but one of the antibiotics tested.
Bacteria do not respect borders, and the widespread resistance emergence in S. epidermidis poses a threat to several routine practices such as drawing blood from patients and, naturally, surgery.
The role of hospital practices and antibiotic stewardship in preventing the spread of resistant bacteria is of paramount importance, but it's equally important medical practitioners should be made aware of these findings, so they can make better decisions in prescribing antibiotics to their patients.



 Australia; VIC
Australia; VIC