Media release
From: Kirby Institute, UNSW SydneyKey findings
- In 2021 there were 86,916 diagnoses of chlamydia, 26,577 of gonorrhoea and 5,570 of infectious syphilis in Australia.
- There were reductions in total chlamydia and gonorrhoea diagnoses nationally – but also a drop in the numbers of Australians having a test for sexually transmissible infections (STI) (14% down from pre-pandemic levels for chlamydia and gonorrhoea tests) – impacted largely by the COVID-19 pandemic.
- In contrast infectious syphilis diagnoses increased in 2021, after having fallen between 2019 and 2020. There have been steady rises in infectious syphilis among gay and bisexual men and among Aboriginal and Torres Strait Islander people.
- There were increases in the number of infectious syphilis diagnoses among women of reproductive age. In the same time period, there has been a large increase in the number of congenital syphilis diagnoses, with a disproportionate number occurring among Aboriginal and Torres Strait Islander babies.
- According to modelling, most chlamydia gonorrhoea cases remain undiagnosed and untreated.
- Among Aboriginal and Torres Strait Islander people, rates of gonorrhoea and infectious syphilis were more than five times as high, and rates of chlamydia diagnosis were almost three times as high, compared with non-Indigenous Australians. This disparity is much greater in remote areas of Australia.
- There continue to be high rates of chlamydia, gonorrhoea and syphilis diagnosed among gay and bisexual men living in major cities.
- Reflecting the success of the national HPV vaccination program, diagnoses of genital warts among heterosexuals aged under 21 attending sexual health clinics declined to less than 1% among females and 0% among males under 21 years.
- There were no reported diagnoses of genital warts in 2021 among Aboriginal and Torres Strait Islander peoples aged under 21 years attending sexual health clinics.
(SYDNEY, Thursday 8 December 2022) New data released today by the Kirby Institute at UNSW Sydney reveals how the COVID-19 pandemic has impacted testing and diagnoses of sexually transmissible infections (STI) in Australia.
The report titled HIV, viral hepatitis and sexually transmissible infections in Australia: Annual surveillance report shows that in 2021 there were 86,916 diagnoses* of chlamydia, 26,577 of gonorrhoea and 5,570 of infectious syphilis in Australia.
“Prior to the pandemic we were seeing increases in chlamydia and gonorrhoea, but in 2021 we recorded a small decline. We believe this reduction is a consequence of both reduced testing and reduced sexual activity with new or casual partners, due to social restrictions and lockdowns during 2020 and 2021,” says Dr Skye McGregor from the Kirby Institute, one of the report’s authors. “On the other hand, syphilis has been steadily increasing among women of reproductive age, gay and bisexual men and Aboriginal and Torres Strait Islander people. This reflects sustained and ongoing transmission across Australia, which is extremely concerning."
Most STIs remain undiagnosed: Test, Test, Test
According to modelling in the report, most chlamydia and gonorrhoea cases in Australia remain undiagnosed and untreated, highlighting a need to increase STI testing across the country. More than one in 25 young people aged between 15-29 in Australia had chlamydia during 2021 but less than a third of those young people received a chlamydia diagnosis.
“People with chlamydia and gonorrhoea, the most common notifiable STIs, often don’t have any symptoms. But these STIs can still be passed on to others and cause serious long-term health concerns like pelvic inflammatory disease in women and infertility in men and women. This is why regularly testing, and treatment is crucial for STI control. But based on Medicare testing data, between 2019 and 2021, the number of people aged 15 to 24 years getting a chlamydia or gonorrhoea test declined by 14% in Australia. It’s important we encourage people who have deferred or interrupted their sexual health care to get tested,” says Dr McGregor.
The frequency of testing depends on your risk behaviour, says Professor Basil Donovan who is a sexual health physician and heads up the Sexual Health Program at the Kirby Institute. “The best thing to do is to have a chat with your GP, nurse or health worker about your sexual activity, and they’ll recommend anything from 3-monthly to annual testing. Chlamydia and gonorrhoea are tested for using a simple urine test or a self-collected vaginal swab. It’s also a good idea to get a blood test for syphilis and HIV at the same time.”
Concern over multiple syphilis outbreaks
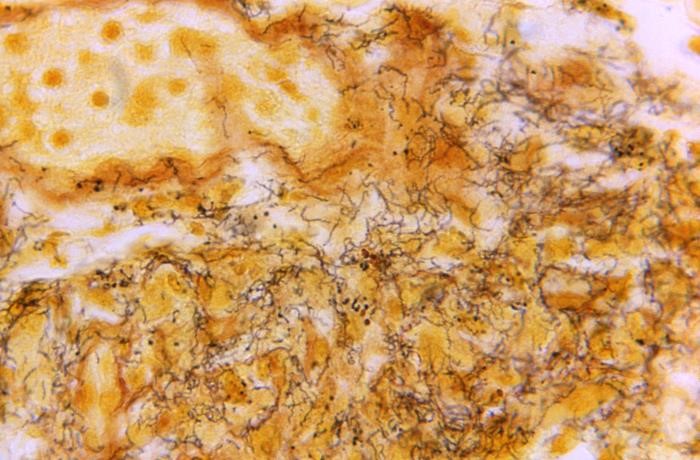
Syphilis diagnoses have been increasing in Australia since 2011, initially with outbreaks among gay and bisexual men in cities and among Aboriginal and Torres Strait Islander people in regional and remote areas of central, northern, and western Australia.
The report also reveals a dramatic increase in syphilis among women of reproductive age in both Aboriginal and Torres Strait Islander women (four-fold) and non-Indigenous women (eight-fold), over the ten-year reporting period.
"While the numbers among women in cities are still relatively small, the upward trend in this group over the last 10 years has been substantial. We are particularly concerned about syphilis in women aged 15-44 years due to the potential impact on pregnancy outcomes. The data tell us that we may need to focus on enhanced sexual health messaging about syphilis for all sexually active people who may be at risk, and ensure appropriate education for health providers," says Dr McGregor.
Congenital syphilis occurs when syphilis is transmitted during pregnancy to an unborn child. Between 2012 and 2019, diagnoses were low, ranging from 0-8 each year. In 2020 and 2021 there were 17 and 15 congenital syphilis diagnoses, respectively, representing a considerable increase. In 2021, 60% of congenital syphilis diagnoses were among Aboriginal and Torres Strait Islander babies, who make up only approximately 5% of newborns.
“This is particularly worrying, as pregnant women should be tested regularly for STIs as part of pre and antenatal health screening, but COVID-19 has put additional strains on health service delivery and access. With timely screening, syphilis can be cured, so even one case of congenital syphilis is completely avoidable and unacceptable. At the Kirby Institute, we’re working with our partners to understand what proportion of pregnant women are not receiving adequate STI screening,” Dr McGregor said.
Good news for the elimination of genital warts
Diagnoses of genital warts at first sexual health clinic visit are tracked as a marker of infection with human papillomavirus (HPV). In 2021, diagnoses of genital warts among non-Indigenous people aged under 21 years declined to less than 1% among female clinic attendees, or five diagnoses overall, and 0% among heterosexual male clinic attendees, or no diagnoses overall - reflecting the success of Australia’s HPV vaccination program.
STIs remain much higher among Aboriginal and Torres Strait Islander populations, but progress with donovanosis and HPV
In 2021, rates of diagnosis of STIs among Aboriginal and Torres Strait Islander people remained much higher than among the non-Indigenous population, with rates of gonorrhoea and syphilis more than five times as high, and rates of chlamydia more than three times as high.
Mr Robert Monaghan, a Bundjalung-Gumbaynggir man and Manager of Aboriginal and Torres Strait Islander health research at the Kirby Institute, says “these statistics highlight the need for culturally appropriate health promotion, testing and treatment strategies co-designed and delivered in partnership with these populations.”
Mr Monaghan said that the success in driving down other STIs is cause for optimism about what can be achieved working in partnership with Aboriginal communities. “Donovanosis, once a commonly diagnosed STI among remote Aboriginal populations, is now close to elimination, with only two diagnoses since 2012. And the HPV vaccination has been hugely successful, with no diagnoses of genital warts among Aboriginal young people under 21 years in 2021.”
Gonorrhoea and syphilis increasing in gay and bisexual men
While HIV has been declining among Australian-born gay and bisexual men thanks to high coverage of the HIV prevention medication pre-exposure prophylaxis and use of treatment as prevention, gonorrhoea and syphilis diagnoses have been increasing in recent years among this population.
“69% of gonorrhoea diagnoses are among men as are 81% per cent of syphilis diagnoses. From this we can infer that these infections are occurring disproportionately among gay and bisexual men,” says Professor Andrew Grulich from the Kirby Institute.
“Some of this increase may be related to decreases in condom use, which have occurred in an era of greater use of other highly effective biomedical HIV prevention and treatment strategies.”
The number of gay and bisexual men attending sexual health clinics and getting tested for STIs declined between 2019 and 2021. Professor Grulich said that while it made sense that there was a reduction in testing during the pandemic when people were having less casual sex, “as people return to their pre-pandemic sexual behaviours, it is important to return to regular STI testing."
“We’ve had tremendous success in HIV prevention. We need to carry this over to STIs, to drive down infections among this group.”
* The report analyses notifications data from the Australian National Notifiable Diseases Surveillance System. Diagnoses of certain conditions in Australia are notifiable to state and territory health authorities. The term diagnoses has been used instead of notifications for simplicity.