News release
From:
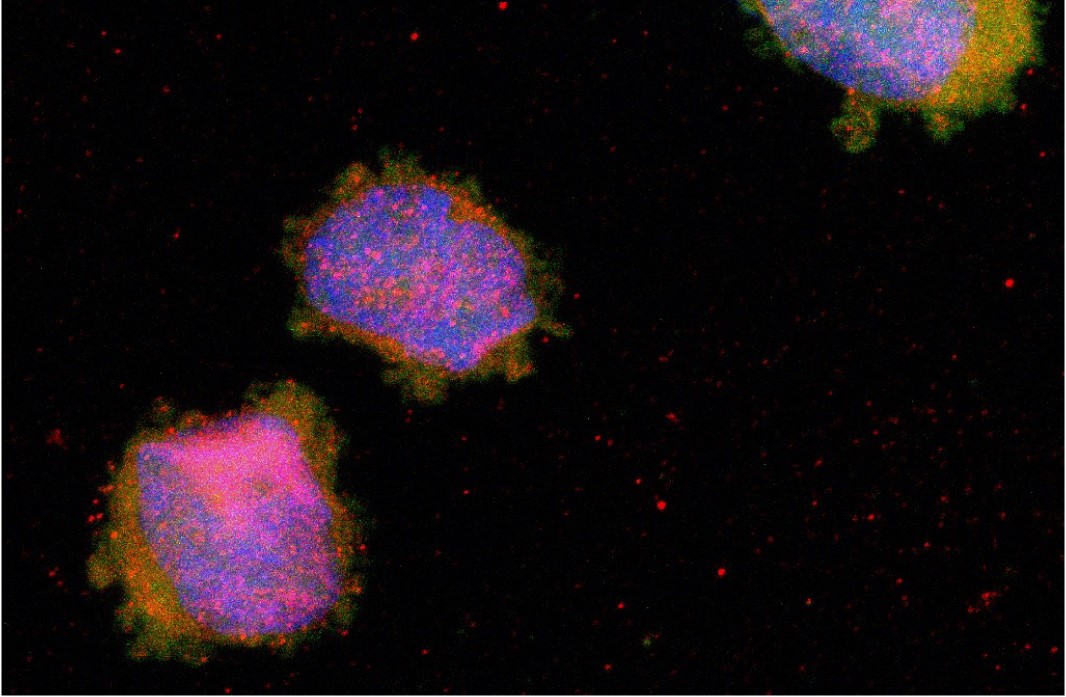
Researchers at Peter Mac have discovered a new way to kill cancer cells in acute myeloid leukaemia (AML), one of the most aggressive and hard to treat forms of blood cancer.
The team found that AML cells, especially stem cells that drive relapse, rely on a common molecule called heme to survive and keep multiplying.
When this process is blocked, the cancer cells die through a newly identified form of cell death known as cuproptosis.
“We’ve uncovered a fundamental weakness in AML cells,” said Dr Alexander Lewis, Postdoctoral Researcher at Peter Mac.
“By blocking AML cells from producing heme, we can switch on cuproptosis, a unique form of cell death, and effectively kill the cells most responsible for causing a cancer relapse.
“This opens the door to new therapies that are potentially more powerful and longer lasting.”
Around 900 Australians will be diagnosed with AML every year with half of all patients relapsing after remission.
The prognosis patients who relapse after treatment is currently very poor with the median survival between four and six months.
“This discovery could lead to new treatments that not only kill AML cells but also prevent the disease from coming back after initial therapy,” Dr Lewis said.
“Importantly, this approach may be effective even in AML that has become resistant to standard drugs.”
The study also identified other metabolic pathways that could be targeted in combination with heme-blocking strategies, offering the potential for even more effective treatments in the future.
While more work is needed before this discovery can be tested in clinical trials, the findings mark an important step towards giving AML patients new hope, especially those with drug-resistant disease.
This research was published in Cell and was conducted in collaboration with the WEHI, Florey Institute, Monash University, Murdoch Children’s Research Institute and the Centre for Cancer Biology.



 Australia; VIC; SA
Australia; VIC; SA