News release
From:
Neurodegeneration: Further evidence for the transmission of amyloid beta pathology (N&V) *PRESS BRIEFING*
Specific batches of cadaveric human growth hormone (c-hGH) samples were contaminated with amyloid beta protein, reports a paper published online in Nature this week. These samples were able to subsequently seed amyloid beta pathology in mice. A previous paper suggested c-hGH as a possible source of amyloid beta pathology in four patients that had received c-hGH as treatment for short stature. Although these new findings do not demonstrate the direct transmission of Alzheimer’s disease, they provide experimental evidence that the c-hGH the patients received is able to transmit amyloid beta pathology.
A Nature paper published in 2015 reported the presence of amyloid beta pathology in the brains of four out of eight patients who had received prion-contaminated c-hGH and subsequently died of Creutzfeldt–Jakob disease (CJD). Amyloid beta pathology is a hallmark of cerebral amyloid angiopathy (CAA) and Alzheimer’s disease. Several of the patients displayed pathology resembling CAA; however, none met the full neuropathological criteria for Alzheimer’s disease. Although the human transmission of CJD as a result of certain medical procedures (iatrogenic transmission) had been previously documented, this study suggested that the patients may have developed amyloid beta pathology from the treatment with c-hGH. However, further investigation was required to determine whether the c-hGH samples were contaminated with amyloid beta.
Following on from this previous work, John Collinge and colleagues obtained several of the c-hGH samples that the patients had been exposed to. These were analysed biochemically for the presence of amyloid beta and tau protein, and a number of samples tested positive for both.
Next, the authors investigated whether the amyloid beta protein found in the samples had the potential to seed amyloid beta pathology in live organisms. c-hGH samples were administered to genetically modified mice, which express a mutated, humanized version of the amyloid precursor protein (APP) gene and develop the first signs of amyloid beta deposition at around six months of age. Female mice aged 6–8 weeks received injections of the original c-hGH samples directly into the brain. At 240 days post-injection, amyloid beta deposits and CAA were consistently found in mice that received the original c-hGH samples, but were almost completely absent in various control mice (including those that received currently used synthetic recombinant hGH). The authors highlight that the seeding potential of the tau detected in the c-HGH samples requires testing in a separate tau mouse model.
These findings demonstrate that the original c-hGH batches contained amyloid beta that is able to seed amyloid beta pathology in mice, and provides experimental evidence to support the hypothesis that amyloid beta pathology can be transmitted to humans by iatrogenic means. The authors emphasize that there is no suggestion that Alzheimer’s disease is a contagious disease or transmissible by blood transfusion, although they state that it is important to evaluate the risks of iatrogenic transmission of amyloid pathologies.
**Please note that a telephone press briefing will take place UNDER STRICT EMBARGO on Wednesday 12 December at 1500 London time (GMT) / 1000 US Eastern Time.**
Author John Collinge will discuss the research. This will be followed by a Q&A session.
To attend this briefing you will need to pre-register by following the link here. Once you are registered, you will receive an email containing the dial-in details for the conference. You will also be provided with the option to save the details of the briefing to your calendar.
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Dr Ian Musgrave is a Senior Lecturer in the Faculty of Medicine, School of Medicine Sciences, within the Discipline of Pharmacology at the University of Adelaide.
Alzheimer’s disease is the major dementing disease in Australia and the world, taking a terrible toll on patients and their families.
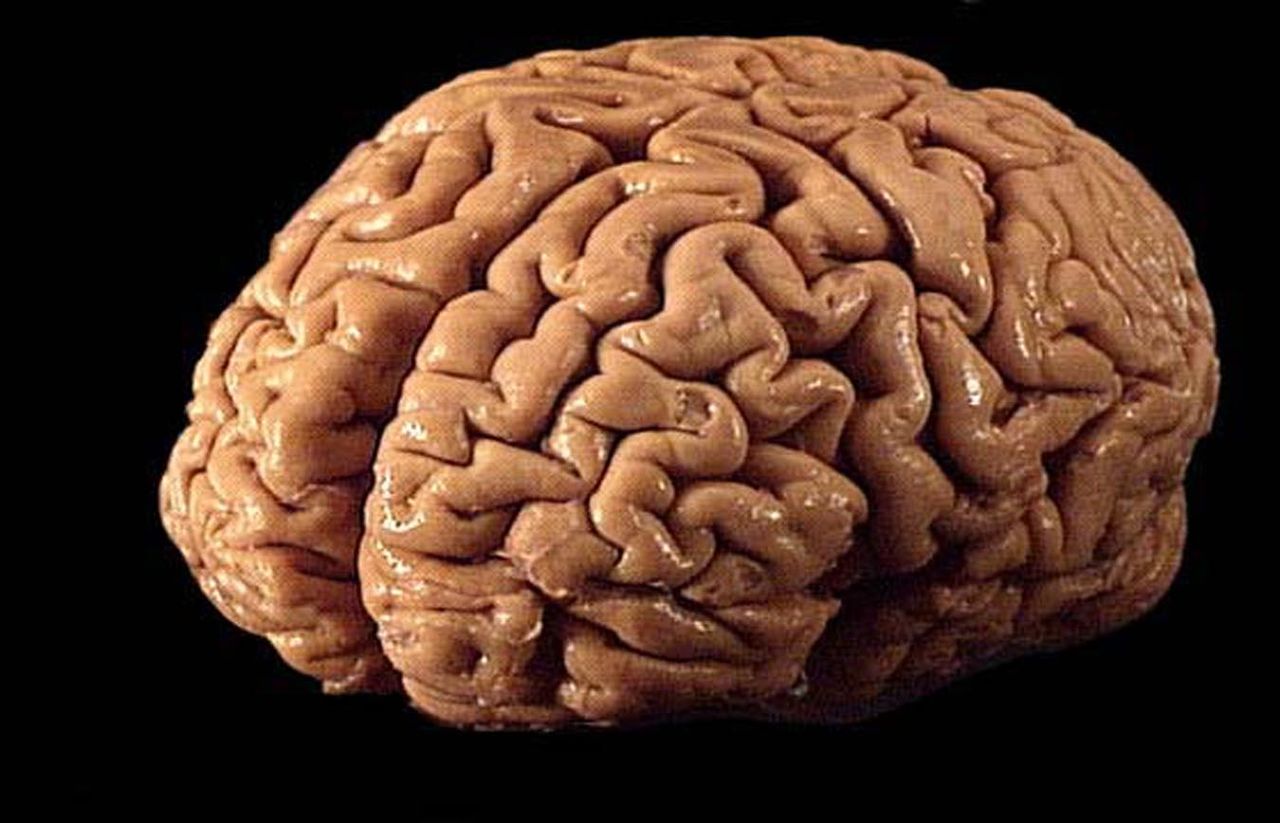
One of the hallmarks of AD is the accumulation of an insoluble protein in the brain, beta amyloid. Beta amyloid is toxic to brain cells, and is thought to be important in the development of AD, yet every therapy we have thrown at AD based on removing amyloid has failed, prompting a rethink of its importance.
These new finding bring beta amyloid back into the spotlight. We have known the beta amyloid is a prion like protein for some time. Prion proteins are responsible for diseases such as Kuru, Creutzfeldt-Jackob disease and “mad cow” disease. Prion proteins are misfolded, toxic versions of normal proteins that can act as seeds causing the normal proteins to misfold into the toxic versions in a slow but lethal cascade.
While beta amyloid has prion-like properties, this was considered largely irrelevant to AD (as we don’t eat the brains of our elderly).
In this recent work researchers have isolated beta amyloid from vials of human growth hormone derived from human cadavers that were given to people who later developed an AD like disease. Injecting these beta-amyloid containing preparations into the brains of mice that have been genetically modified to express human beta amyloid caused them to develop the same AD like disease.
This suggests that beta-amyloid does play a central role in the development of AD, and we now must investigate why anti-beta amyloid therapies have failed more closely.
Dr Bryce Vissel is a Professor in the School of Clinical Medicine at UNSW and Director of the Centre for Neuroscience and Regenerative Medicine at St Vincent's Hospital Sydney
The study suggests that amyloid beta, when present as a small contaminating substance in preparations of hormones given to children over the period 1958-1985, can seed amyloid plaques in the brain of mice. While interesting scientifically this study has no implications for children or adults taking hormone preparations today. This is because hormones are prepared today in a very different way now, compared to how hormones were prepared in 1958-1985. The hormone in those days was prepared from the brains of cadavers, so the hormone preparation was not pure as it is today where it is made by more sophisticated methods.
This study is of interest scientifically because it shows that amyloid from those very old preparations of contaminated hormone, when injected into brains of mice, can seed increased amyloid deposition in mice. Therefore the study suggests, but does not prove, that that amyloid can act as a kind of infectious agent: the amyloid in the contaminated hormone preps could possibly have been the cause of the cerebral amyloid angiopathy and plaques seen in some humans that received the contaminated hormones twenty or thirty years earlier.
More details:
Growth hormone was once prepared by extracting it from the brains of cadavers and then was given to children that needed growth hormone. The hormones prepared this way were of course not absolutely pure and some of the batches contained small amounts of amyloid. Some children receiving batches of the contaminate hormone in 1958-1985, went on to develop evidence of mild cerebral amyloid angiopathy and plaques 20-30 years later, though this did not meet the criteria for Alzheimer’s disease.
In this study, old contaminated batches of the hormone from 1958-1985 that were pulled out from the freezer, were able to seed cerebral amyloid angiopathy and plaques in mice that were genetically predisposed to get these plaques. It is important to note however that first, the preparation was directly injected into the brains of mice, while in humans it was given as an injection into the blood. Second, the mice were genetically predisposed to develop angiopathy and plaques. Third, in the humans, only mild cerebral amyloid angiopathy and plaques were seen 20-30 years later, which did not meet the criteria for Alzheimer’s disease.
So this study shows that the amyloid from the contaminated hormones are able to seed plaques and provides suggestion, but does not prove, that amyloid in the contaminated hormones were the cause of the cerebral amyloid angiopathy and plaques in the humans. However given hormones are prepared very differently today, this is not relevant for anyone taking hormones today.



 International
International