News release
From:
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Professor Garry Jennings AO is the Heart Foundation’s Chief Medical Advisor, the Executive Director at Sydney Health Partners, Senior Director at Baker IDI Heart and Diabetes Institute, and a cardiologist with Alfred Health
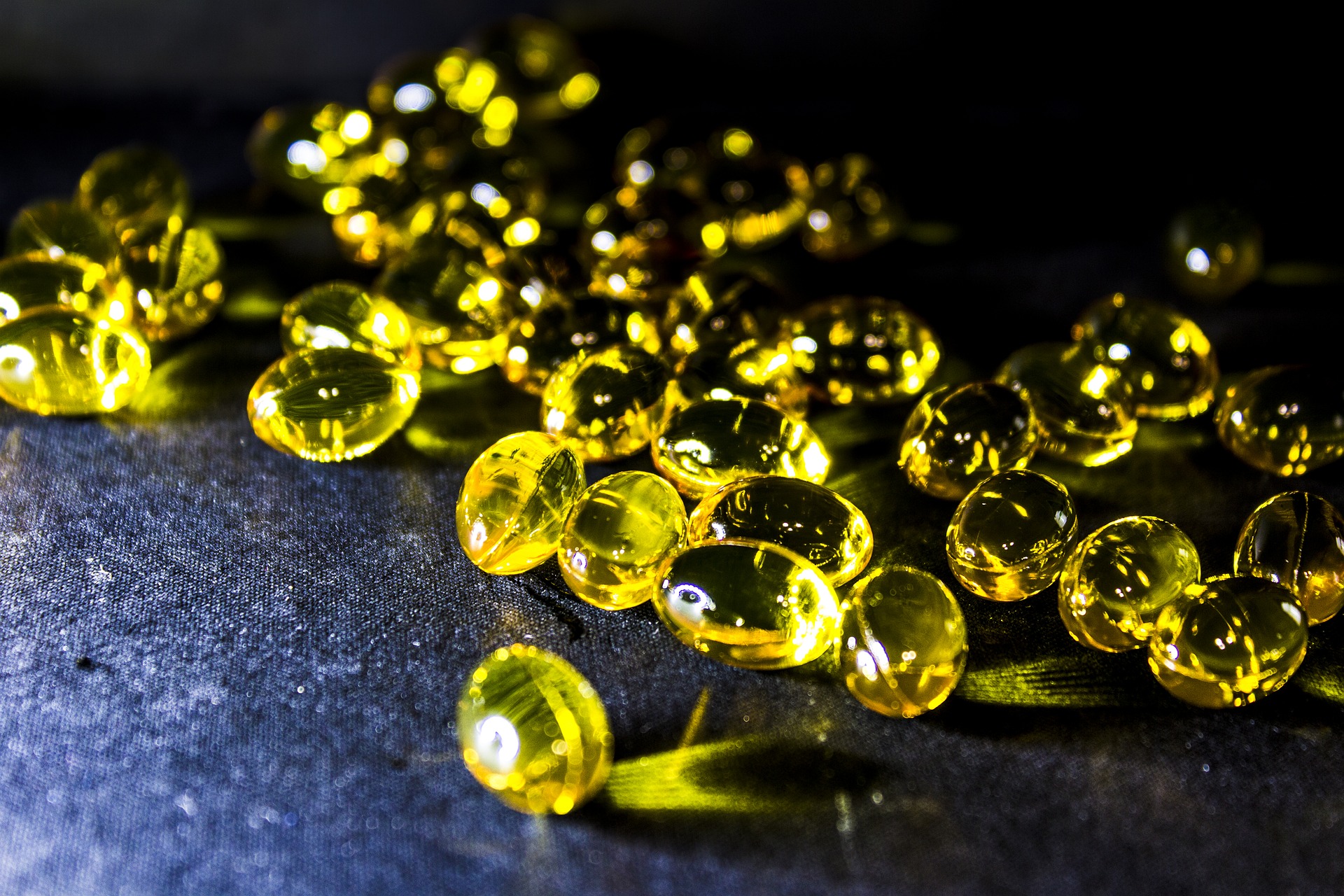
This is a meta-analysis investigating the links between omega 3 fatty acid supplements and the risk of coronary heart disease and stroke in people who have a history of coronary heart disease.
The study found that omega 3 supplementation did not have either a beneficial or adverse effect on people who already had coronary heart disease.
This aligns with the Heart Foundation’s current position that the evidence has changed for omega-3 supplements.
The results of this meta-analysis align with the Heart Foundation’s current recommendations;
· we do not advise routine recommendation of omega-3 supplements for heart health by health professionals
This meta-analysis did not assess the role of fish in a healthy eating pattern, and so does not affect current recommendations to include 2-3 serves of fish per week as part of a heart healthy diet.
David Sullivan is Head of Chemical Pathology at the Royal Prince Alfred Hospital, and is also from Health Pathology from NSW Government
The group responsible for the JAMA paper are very capable and well regarded. Their analysis involves a different window of time. Results from additional studies are anticipated in the near future and some of those studies have involved higher doses of omega 3 supplements.
One possible explanation is that studies have never attempted to recruit appropriate patients by way of assessment of their omega 3 nutritional status – perhaps omega 3 supplements only work in subjects who have a low “omega 3 index” as measured by their red blood cell fatty acid composition. It is important to note that omega 3 supplements do not improve LDL cholesterol levels, which are a strong indicator of CVD risk. On the other hand it is possible that fish consumption and/or omega 3 supplementation could have less well-proven benefits on CV function including reduction in plasma triglyceride levels.
Craig Anderson is Head of Global Brain Health at The George Institute and Professor of Neurology and Epidemiology at UNSW Sydney. He is also a Neurologist at Royal Prince Alfred Hospital.
This is an important research publication providing a reliable assessment of the totality of the evidence from large, long-term, randomised trials for any treatment effect of omega-3 (fish oil) consumption and serious cardiovascular events. The results show no evidence of any beneficial effect for the secondary prevention of cardiovascular disease events in high risk adults.
Personally, I find this evidence not too surprising. 1-3 tablets of fish oils has no effect on lipid levels, coagulation or platelet function, and the fish oil loses potency through natural oxygenation within a few months after opening the cap (hence, fish oil smell).
While not the focus of this paper, there is evidence to support use of a very high dose of fish oils (up to 20 tablets per day) for modification of lipid levels (but statins and other pharmacological treatments are simpler, more effective and preferable in those with familial hyperlipidaemia) and stabilising heart rate in those with an irritable or irregular heart rhythm.
Use of fish oils is widely promoted as having magic health benefits but the science to support this based on the highest levels of research are very limited.
Professor Mark L Wahlqvist AO is Emeritus Professor and Head of Medicine at Monash University and Monash Medical Centre. He is also Past President of the International Union of Nutritional Sciences
As useful as this large negative meta-analysis of n-3 fatty acid supplements and cardiovascular disease is for consumers, it should not be over-interpreted. Negativity is not proof.
Populations not studied may benefit: Asians handle n-3 fatty acids differently to Europeans. Not all n-3 fatty acids are the same. More information about adverse effects should be provided along with ‘no detectable effect’.
It is not a study of food, like fish and plant sources of n-3 fatty acids of various chain lengths, with their complex bioactive components, interactive with n-3 fatty acids.
Earlier studies reported in this study antedated the growing contamination of seafood with microplastic and endocrine disruptors, which may compromise the benefits of n-3 fatty acids. It does not take into account the background diet.
Last, but not least, the benefits of supplementation in replete individuals will not be the same as in deficient individuals- less people are now deficient in food culturally aware societies. This means other health domains like diabetes, brain function and bone health may have different outcomes in accord with n-3 fatty acid intakes.
Professor Rachel Huxley is Associate Pro Vice-Chancellor (Academic Partnerships) in the College of Science, Health and Engineering, La Trobe University
If you are one of thousands of Australians regularly consuming a fish oil tablet in the belief that you are reducing your risk of having a heart attack then it appears that you are wasting your money.
Findings from the largest and most reliable study to date have shown that consuming a small amount of fish oil in tablet form does not provide any benefit in terms of lowering a persons’ risk of having a heart attack.
As with many vitamin supplements, popping a fish oil tablet is no substitute for eating healthily and living well.
Dr Yutang Wang is a Senior Lecturer in the School of Applied and Biomedical Sciences, Faculty of Science and Technology, Federation University Australia
Omega-3 fatty acids are essential for normal function of our body. Our body cannot make these fatty acids and needs to obtain them from food including fish and fish oil.
Some studies showed that omega-3 fatty acid supplement may help to prevent cardiovascular events such as heart attack, stroke, or even death. However, results are contradicting. Some studies showed that the supplement had no beneficial effect, and even a small number of studies found that taking the supplement might do us harm.
This newly published meta-analysis of 10 high-quality clinical trials involving about 80,000 people showed that omega-3 supplement did not protect us from cardiovascular disease at all. Therefore, we may need to rethink the usefulness of taking the supplement.
The American Heart Association recommends the use of the supplement in patients with existing coronary heart disease. However, evidence for this recommendation is not very strong. More research is needed to find out who is likely to benefit from taking the omega-3 supplement.
In addition, some researchers are currently trying to find out whether a higher dose of omega-3 (e.g. 3-4 g per day versus ~1 g per day used in most studies) will provide any benefit.
Professor Barbara Meyer is the Director of the in the Lipid Research Centre in the School of Medicine at the University of Wollongong
Using the correct dose of omega-3, docosahexaenoic acid (DHA) may help.
The dose of omega-3, DHA, is too low – hence the lack of benefit seen for heart health seen in the recent meta-analysis by Aung et al.
The ten studies used in this meta-analysis: most studies were underpowered (one study called DOIT was designed as a primary prevention trial but it only had 563 participants – therefore it is definitely under-powered to show an effect) and they had lower than expected event rates.
Only 2 studies used the correct dose of omega-3, particularly 0.5g of DHA per day. These 2 trials that used the correct dose of DHA are the GISSI-HF and GISSI-P trials and these 2 trials are in favour of omega-3 having benefit for coronary heart disease death (figure 2 in publication Aung et al.).
The other trials did not use a high enough dose of DHA (i.e. 0.5g DHA per day – see graph) to show benefit for heart health. Please note that the JELIS trial used omega-3 eicosapentaenoic acid (EPA) and not DHA. It is DHA that has the anti-arrhythmic effect and therefore prevents sudden cardiac death.
Only 2 studies measured omega-3 in the blood and due to the low supplemental dose, the omega-3 levels only increased by 1%, which is not high enough to see any benefit.
Associate Professor Michael Skilton is a Future Leader Fellow and Program Leader at The Boden Institute of Obesity, Nutrition, Exercise & Eating Disorders, The University of Sydney
This study looks at the effect of omega-3 supplements on risk of cardiovascular disease, by combining the data from a number of trials. The results are similar to those from previous similar studies, and show that in older adults with existing heart disease, there is no strong indication that omega-3 supplements are beneficial for preventing future heart attacks or strokes. But the results for death from heart disease were less clear cut, with borderline evidence that omega-3 supplements may be beneficial.
The trials included in the current study had differences in study designs, including the dose of omega-3s given to participants, which may have contributed to the differences in findings between trials.
The addition of results from future trials will hopefully provide more clarity with regards to whether omega-3 supplements are beneficial for heart health. It is worthwhile emphasizing though that these findings specifically relate to omega-3 supplements.
There is strong evidence that omega-3 rich foods, such as fish and walnuts, reduce a person’s risk of developing cardiovascular disease.



 International; NSW; VIC
International; NSW; VIC