Media release
From:
A simple test could predict a newborn’s risk of developing type 2 diabetes
A genetic test of cord blood at birth may hold the key to predicting a child’s future risk of developing type 2 diabetes, according to exciting new research from Australia and Hong Kong.
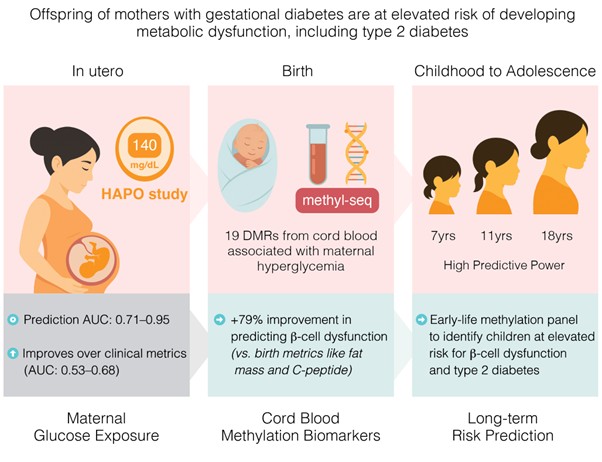
By analysing the DNA in cord blood from babies born to mothers with gestational diabetes or high blood sugar during pregnancy, researchers have identified early epigenetic markers that forecast insulin resistance and beta-cell dysfunction up to 18 years before diabetes develops.
These findings from Australia’s Baker Heart and Diabetes Institute and The Chinese University of Hong Kong offer a major step forward in personalised medicine. The study was co-led by Professor Sam El-Osta, head of Baker Institute’s Epigenetics team, and Professor Ronald Ma from The Chinese University of Hong Kong. Professor Sam El-Osta says, “This research points to a future where we can identify a newborn’s risk of type 2 diabetes at birth and take steps immediately to reduce that risk. It changes the way we think about when, and how early, we can intervene to prevent chronic disease in childhood.
“We know children born to mothers with gestational diabetes during pregnancy face a greater risk of developing metabolic disorders like type 2 diabetes later in life. Until now, identifying which children are most at risk has been difficult, and existing tools - such as birth weight, fat mass or cord blood insulin - have been limited in their ability to predict the development of the disease.”
The study showed the epigenetic signatures in cord blood improve prediction of beta cell dysfunction by 79% compared to traditional clinical markers used in adult testing like fat mass or C—peptide.
This study, published today in the Diabetes Journal, offers the first longitudinal demonstration that epigenetic markers found in cord blood can be used to assess lifelong diabetes risk. After assessing children and young people aged 7, 11, and 18 years, we have found that as well as predicting risk of type 2 diabetes as early as birth, this technique can be relied upon as a strong predictor through childhood to adolescence.
Australian Diabetes Society CEO, A/Prof. Sof Andrikopoulos says, “This study significantly progresses our understanding of how high blood glucose during pregnancy can predispose children to future risk of diabetes. By knowing the children that are at highest risk of diabetes, we can provide the appropriate care and education early in life to prevent the onset of diabetes in adulthood to lessen the burden on the health system.”
These findings pave the way for personalised prevention programs, such as lifestyle or dietary adjustments from early childhood, allowing action decades before disease onset. This cord blood test could become part of neonatal screening panels and inform protective strategies from early childhood to reduce metabolic dysfunction and diabetes risk long before the disease develops.
This research reveals our preventative care should begin even earlier, as Professor El-Osta explains. “The study shows mothers who have glucose levels below what is currently diagnosed as gestational diabetes can pass on this metabolic risk to their babies. This suggests implications for much earlier screening and intervention.”
Mothers are currently screened for gestational diabetes during their pregnancy. If mothers are found to have high blood sugar, we could better support mothers throughout pregnancy to lower their glucose and help reduce the risk for the next generation. This study also highlights the need for stronger education programs emphasising healthy diet and lifestyle throughout pregnancy to reduce the risk of developing high blood sugar.
Researchers are hoping to conduct further clinical trials before looking to commercialise and translate this simple test into clinical practice.
About type 2 diabetes and epigenetic markers
Type 2 diabetes is a condition that has strong genetic and family-related (non-modifiable) risk factors and is also often associated with modifiable lifestyle risk factors. It is a condition in which the body becomes resistant to the normal effects of insulin and gradually loses the capacity to produce enough insulin in the pancreas. As a result, the pancreas responds by producing greater amounts of insulin. As insulin overproduction occurs over a long period of time, the insulin-producing cells in the pancreas wear themselves out. This means type 2 diabetes is a combination of ineffective insulin and not enough insulin.
Epigenetic markers are like ‘notes’ on our DNA that don’t change the genetic code itself but influence how and when genes are turned on or off. These changes can happen due to factors like diet, stress, or blood sugar levels during pregnancy.



 Australia; VIC
Australia; VIC