News release
From:
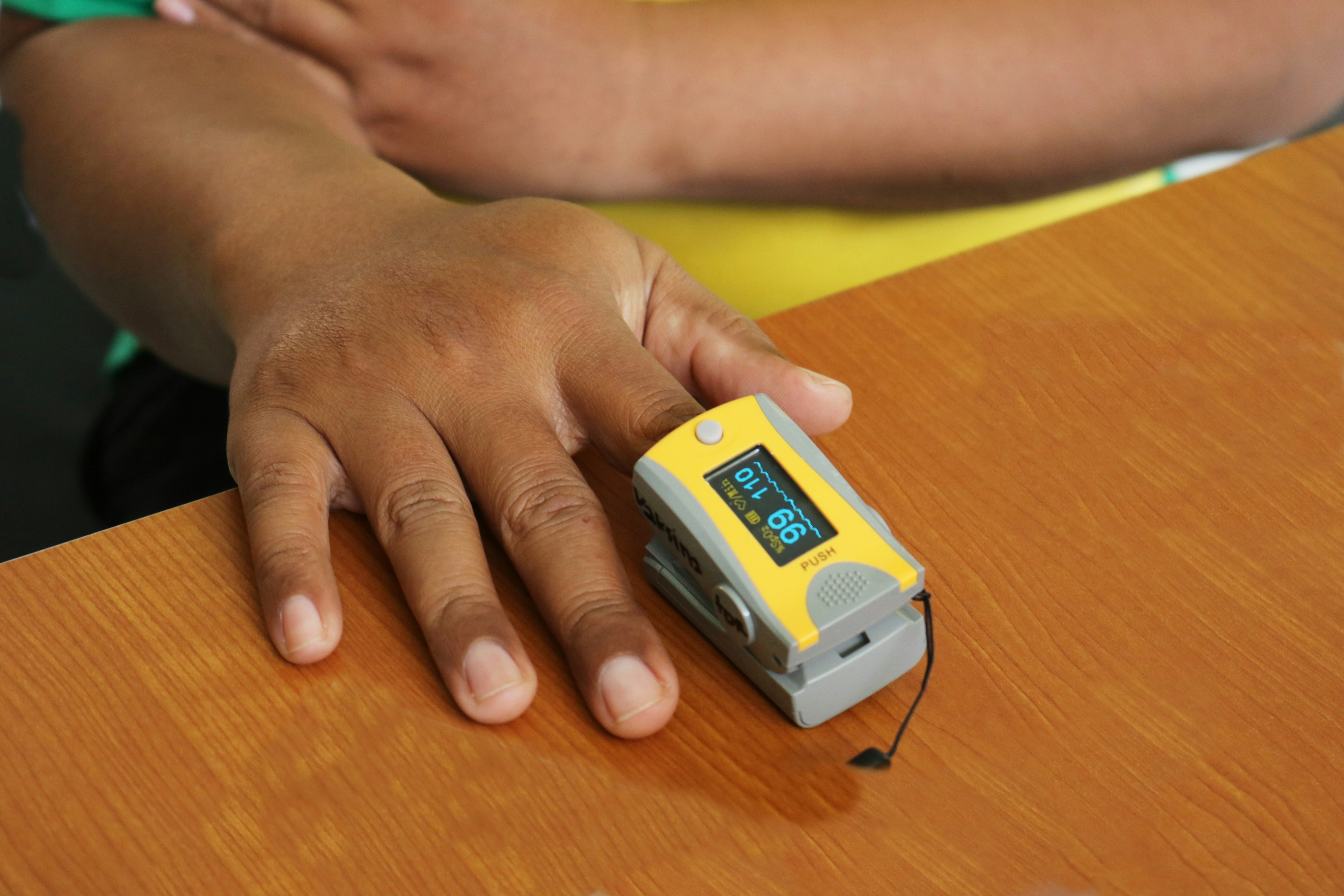
Home fingertip oxygen monitors less accurate for people with darker skin tones
Largest study on this topic suggests that measurement errors lead to potential delays in care and contribute to health disparities
Fingertip monitors known as pulse oximeters that can be used at home to detect low blood oxygen levels (hypoxaemia) give higher readings for patients with darker than lighter skin tones, finds the largest study on this topic published by The BMJ today.
This means that low blood oxygen levels may be missed in patients with darker skin tones, potentially delaying care, while patients with lighter skin tones may get unnecessary treatment.
Pulse oximeters use light to measure the amount of oxygen in the blood (SpO2). For most people, a normal pulse oximeter reading is between 95% and 100%, with readings below 90-92% generally considered low and requiring medical attention.
They are known to be affected by several factors, including skin tone, as pigment in darker skin can absorb more light, making the device “think” there's more oxygen than there is. But so far, studies have been unable to draw any firm conclusions about the impact of skin tone on diagnostic accuracy.
To address this, researchers set out to test the measurement and diagnostic accuracy of five fingertip pulse oximeters provided by the NHS for use at home in the NHS England COVID oximetry @home scheme.
They drew on data from 903 critically ill adults (average age 56 years; 67% male) on 24 NHS intensive care units in England between June 2022 and August 2024.
Although the fingertip pulse oximeters tested were those used at home, intensive care units were used as the test laboratory as patients have lower blood oxygen values and routinely have their blood oxygen accurately measured using hospital machines.
For each patient, skin tone was measured objectively using a spectrophotometer (a type of camera that measures colour). The researchers then compared pulse oximetry blood oxygen values (SpO2) with “gold-standard” arterial blood gas measurements (SaO2).
SpO2 values were assessed at two thresholds in line with current guidance either to seek medical help (94% or lower) or to attend the emergency department (92% or lower).
A total of 11,018 paired SpO2-SaO2 measurements were analysed. All five pulse oximeters returned higher SpO2 values for patients with darker skin tones than patients with lighter skin tones, at any given level of SaO2 measurement.
SpO2 readings were, on average, 0.6-1.5 percentage points higher for patients with darker than lighter skin tone.
At both SpO2 thresholds assessed, false negative rates (low oxygen missed by the pulse oximeter when present) increased with darker skin tones, while false positive rates (low oxygen indicated by the pulse oximeter when absent) decreased with darker skin tone.
And while absolute differences in readings were small, “they can result in substantially higher rates of false negatives and lower rates of false positives in the diagnosis of hypoxaemia,” note the researchers.
This is an observational study, so no definitive conclusions can be drawn about cause and effect. And the authors acknowledge that the study was conducted in critically ill patients, which may limit the generalisability of the findings.
However, they say this was a large study using sophisticated statistical modelling to assess the performance of the pulse oximeters across multiple domains of both measurement and diagnostic accuracy.
As such, they conclude: “SpO2 readings should be interpreted in the context of other clinical information and trends in SpO2 values given greater importance than single readings, particularly in patients with darker skin tones.”
They add: “Healthcare systems should develop guidance to inform and aid practitioners, patients and the public, particularly in settings where additional clinical readings from other medical measurement devices would not be available.”
In a linked editorial, researchers agree that clinicians must recognise the limitations of current devices and interpret readings for patients with darker skin with care and caution, and they say regulation must now catch up with science to mitigate harm.
“The goal is not to abandon pulse oximetry but to understand its limits and make it equitable, ensuring that the technology designed to measure oxygen does not itself perpetuate inequalities in those who receive it,” they conclude.



 International
International