News release
From:
A new study has shown that risk scores based on our genes and gut bacteria can improve the prediction of diseases such as type 2 diabetes and prostate cancer over traditional risk factors alone.
And when it comes to prediction of a person’s risk of coronary artery disease, type 2 diabetes, Alzheimer's disease and prostate cancer, combining traditional risk factors that are used by doctors today with new technologies that quantify our genetic risk (polygenic risk scores) and gut bacteria (gut microbiome) resulted in the most powerful predictors of common chronic diseases.
The study, led by Dr Yang Liu, is one of the first to look at the combined impact of genetics and the gut microbiome on disease risk and paves the way for a more refined, powerful and personalised approach to disease prediction.
Published today in Nature Aging and based on the data of more than 5670 adults, the study is a collaboration by the Baker Heart and Diabetes Institute, the University of Cambridge and the Finnish Institute of Health and Welfare.
While traditional risk factors typically rely on age, sex, and measurements like body mass index, blood pressure, non-HDL cholesterol and HbA1c, this study highlights how large-scale analysis of a person’s genetics and gut bacteria can improve predictive performance.
In this study, researchers investigated the individual and combined predictive performance of polygenic risk scores, the gut microbiome and traditional risk factors for development of future coronary artery disease, type 2 diabetes, Alzheimer's disease and prostate cancer over a median of ~18 years of follow-up, using the population-based FINRISK 2002 cohort.
The recent emergence of multi-omics means that it is now possible to measure and integrate who classes of biomolecular and cellular factors for the purpose of building multi-omic risk scores.
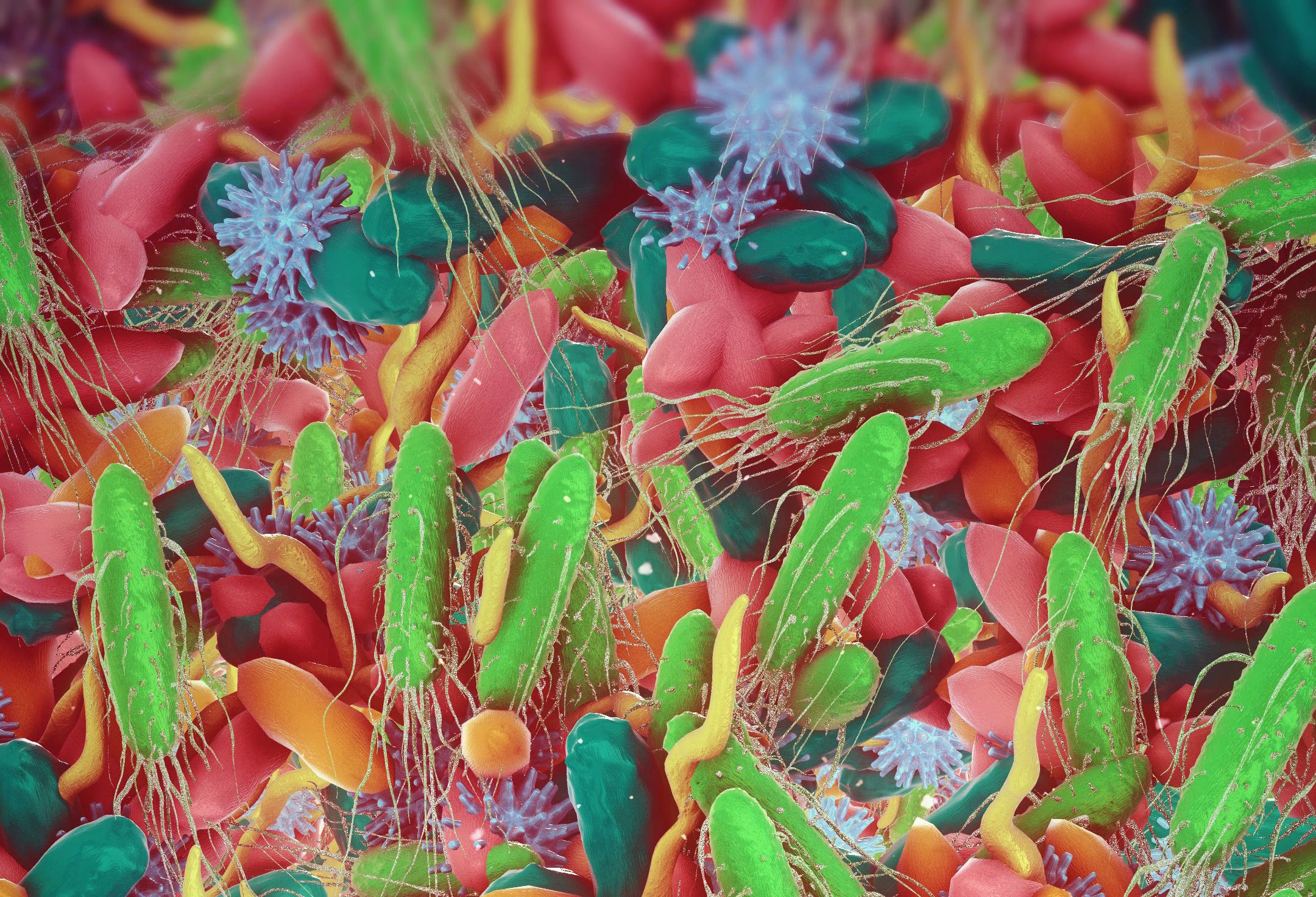
Multi-omic technologies, which are powering discovery across multiple aspects of biology from the genome, proteome and transcriptome to epigenome and microbiome, have uncovered new biomarkers for various common age-related diseases. If diseases such as coronary artery disease, Alzheimer’s Disease, prostate cancer and type 2 diabetes can be predicted early, prevention strategies can also be applied.
Dr Liu says these personalised risk scores, combined with traditional risk factors, open up new avenues for non-invasive risk profiling and early detection of disease.
“This study shows the potential of integrating a person’s multiple omes in advancing understanding of the development and prediction of diseases,” says Dr Liu. “Multi-omics has come a long way, but data integration and translation into benefits for clinical decision-making remain challenging.”
About the Cambridge Baker Systems Genomics Initiative
This work forms part of the Baker Heart and Diabetes Institute's partnership with the University of Cambridge to harness big data to target approaches in disease prediction and personalised medicine. Last year, the Baker Institute announced an extension of the Cambridge Baker Systems Genomics Initiative to 2030 which will build on the Institute's exciting work in this area.



 Australia; VIC
Australia; VIC