News release
From:
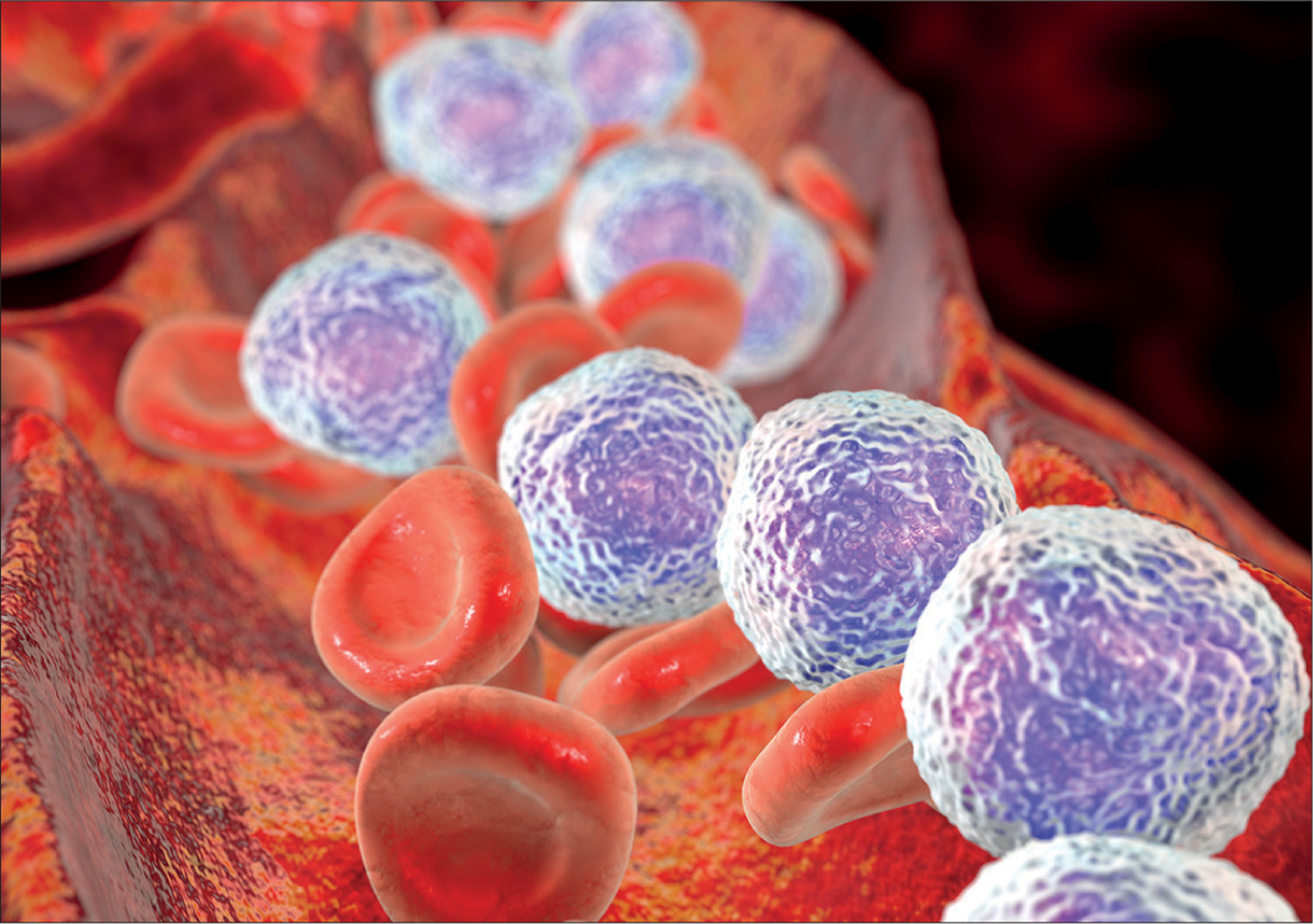
Children with Down Syndrome are 20 times more likely to develop leukaemia and experience more damaging side effects from chemotherapy, but until now science hasn’t been able to pinpoint the reason why.
SAHMRI and University of Adelaide post-doctoral researcher, Dr Elyse Page has found the answer, identifying the epigenetic regulator, HMGN1, on chromosome 21, that cooperates with a high-risk gene fusion to give rise to acute lymphoblastic leukaemia (ALL) in Down Syndrome patients.
“This is an important find not only for children with Down Syndrome, but also children or adults with increased expression of chromosome 21 genes,” Dr Page said Of the total number of children living with Down Syndrome ALL, 60% harbour this high-risk gene fusion, and all have high expression of chromosome 21 genes.
Therefore, they’re extremely prone to developing ALL when the gene fusion arises. Now that the pivotal role of HMGN1 in ALL is understood, it can be targeted for precision treatment to reduce the burden of leukaemia in children with Down Syndrome.
“We’ve already demonstrated an effective targeted therapy which we believe has the potential to reduce the toxic side effects from chemotherapy and improve survival outcomes for children with Down Syndrome ALL,” Dr Page said.
This study presents an opportunity to reduce the overall toxicity leukaemia patients experience from current treatments and improve survival outcomes in this high-risk group.



 Australia; SA
Australia; SA