News release
From:
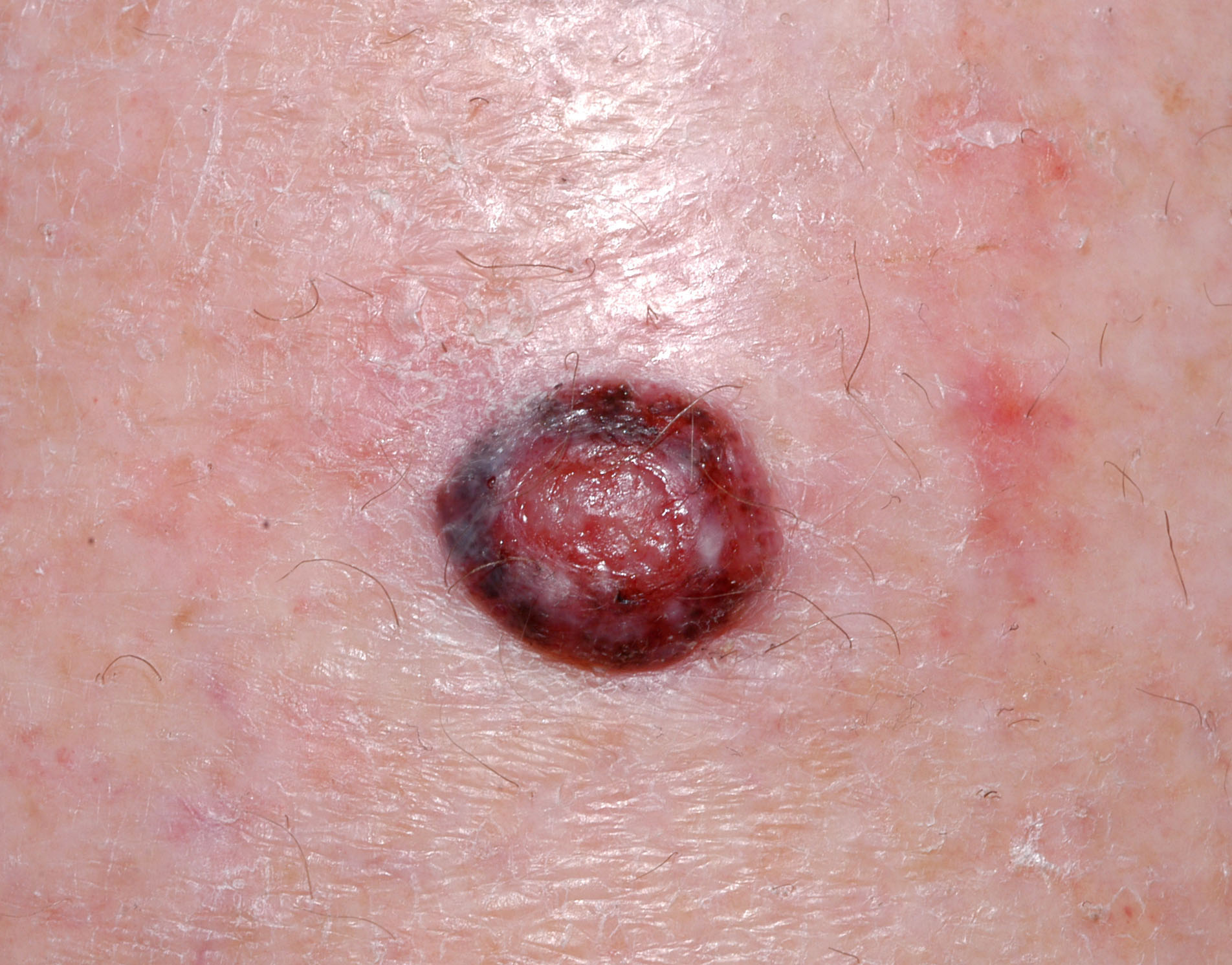
Patient-led surveillance shows promise for melanoma care
Melanoma patients using their smart phone to submit images of lesions to their specialists appears to be a safe and convenient form of follow-up after treatment.
University of Queensland and University of Sydney researchers assessed data from 100 patients who used their phone, had a partner help with skin self-examination and attended regular follow-up visits with a doctor between 2018 and 2020.
Professor Monika Janda, from the UQ Centre for Health Services Research, said the patient-led surveillance group detected five new melanoma cases before clinical visits in the randomized pilot study.
“This suggests the methods used were effective in assisting this group to identify the lesions, while the standard care group did not identify any new melanomas,” Professor Janda said.
“There were three participants with new melanomas found in routine follow-up visits in each group.
“The trial also showed that patient-reporting improved participants’ self-examination knowledge and practices and led to better psychological outcomes.”
The study is part of the University Sydney’s MELSELF project, which is investigating how smartphone technologies can help detect melanomas earlier than usual routine follow-up.
Associate Professor Katy Bell, from the University of Sydney’s School of Public Health, said patient-led surveillance was a new model of follow-up care that allowed melanoma patients to use an attachment on their smartphone to submit images of skin lesions for rapid review by a dermatologist.
“We are currently conducting a larger trial of this same intervention to generate definitive evidence on whether patient-led surveillance can detect new melanomas quicker.”
About 1700 Australians die from melanoma each year and another 500 die from other kinds of skin cancers.
Professor Janda said many melanomas could be self-detected if a person was trained to systematically self-examine their skin and have access to timely review via patient-led surveillance.
“Routine in-person clinic visits are resource-intensive and had not previously been tested compared to patient-led surveillance.
“If confirmed in a larger study, this new model of patient care could reduce clinical visits and the burden on health care systems, and be convenient for people, especially those living further away from treatment centres.”
This study is published in JAMA Dermatology (DOI:10.1001/jamadermatol.2021.4704).



 Australia; New Zealand; NSW; QLD
Australia; New Zealand; NSW; QLD