News release
From:
Cancer: First human trial of CRISPR-edited T cells for personalized cancer treatment
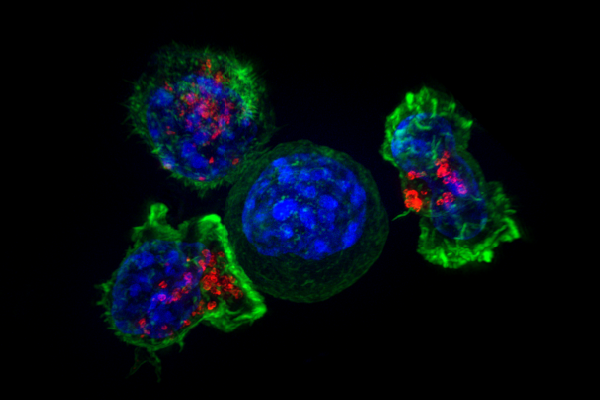
The development and first-in-human clinical testing of non-virally engineered immune cells for cancer therapy is described in Nature this week. The approach, which uses CRISPR genome editing (a system derived from bacteria) to produce patient-specific T cells, had a favourable safety profile. While the clinical benefit in terms of patient responses was limited, the study demonstrates the potential feasibility of this therapeutic strategy.
Harnessing the power of the human immune system is an attractive goal for cancer treatment. Receptors on the surface of T cells (a key part of the immune system involved in the identification of and response to specific antigens) can detect cancer cells because of single mutations in the cancer genome that change cell-surface proteins. Isolating such cancer-detecting T cell receptors and using them to generate therapeutic T cells could provide a new way to treat therapy-resistant cancers.
Antoni Ribas and colleagues developed an approach that uses the CRISPR–Cas9 genome editing system to insert cancer-specific T cell receptors into the T cells of patients with cancer, thereby producing personalized anti-cancer immune cells. In a phase 1 clinical trial, 16 patients with metastatic solid tumours (mostly colorectal cancer) that were resistant to standard therapies were treated with gene-engineered T cells expressing personalized T cell receptors targeting their individual cancer mutations. The treatment resulted in stabilization of disease in 5 of the 16 patients tested, while the other 11 experienced disease progression. Just two patients displayed adverse responses attributed to the T cell therapy, whereas all patients experienced expected adverse effects related to an accompanying chemotherapy treatment.
The authors highlight some limitations to their approach, such as the time needed to characterize potential antigens and to isolate, clone and test T cell receptors, and the different affinities of patient-specific T cell receptors to the associated antigens. They note that some of the processes improved over the duration of the trial and suggest that future improvements are therefore possible.



 International
International