News release
From:
Precision therapy, using insights from how embryos grow, and learning how to thwart zombie cells are three of the ways young Australian researchers are trying to solve some of the most important problems in cancer.
Garvan's Associate Professor Marina Pajic is developing personalised approaches for treating pancreatic cancer, a disease projected to become the second leading cause of cancer death globally by 2030.
She's leading a research program aimed at improving patient survival by matching treatments to individual pancreatic cancers based on the tumour’s ‘molecular fingerprint’
“At the molecular level, pancreatic cancer is not one disease – each cancer is unique and varies significantly from those of other patients and from patient to patient,” Associate Professor Pajic says.
“Currently pancreatic cancer has a dismal five-year survival rate of less than 10% and treatments have not advanced significantly in decades. Through my research, I hope to develop tailored treatment strategies for pancreatic cancer patients and dramatically improve outcomes.”
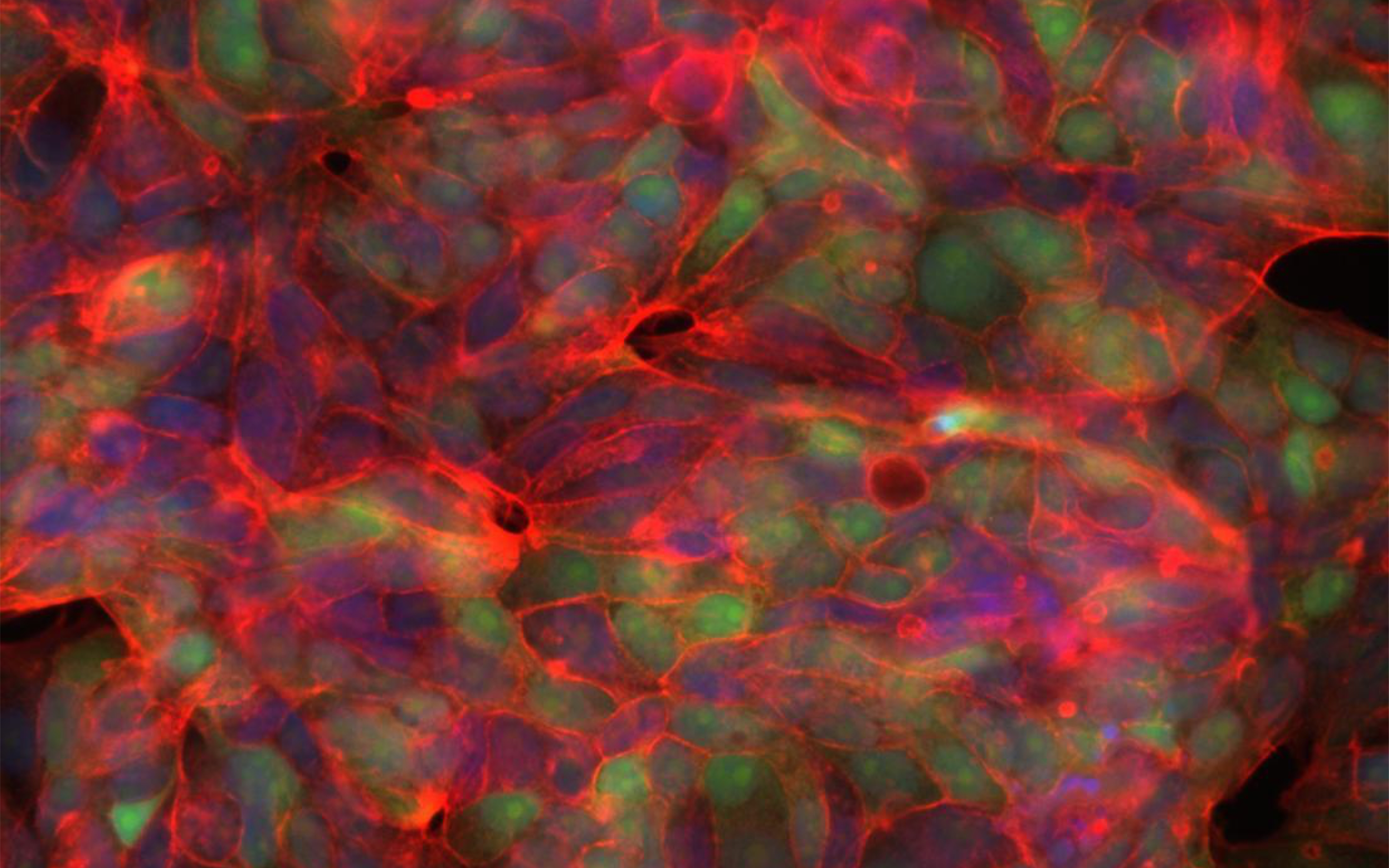
Peter Mac's Dr Melanie Eckersley-Maslin is using insights from how embryos grow to better understand how cancers are caused and develop.
She was previously researching how cell identity and function are established in early development, when she kept on noticing there were lots of similarities between embryology and cancer.
"I had been asking what gives the earliest cells of the embryo the ability to generate all the cell types found in adults – but there is a parallel question no one was looking at about how this normally tightly controlled process is hijacked by cancers," she says.
Dr Eckersley-Maslin believes we can use these lessons from the embryo to discover new targets in cancer, opening exciting new avenues for diagnostics and therapeutics.
The University of Melbourne's Dr Shom Goel is a physician scientist tackling the problem of therapy-induced senescence or, as it is sometimes more colloquially referred to, zombie cancer cells.
“Unfortunately, some cancer cells don’t die in response to common treatments such as chemotherapy or radiation therapy. Rather they enter a state known as senescence and these senescent cells can fuel a cancer’s growth over time, ultimately threatening a patient’s life,” Dr Goel says.
"I want to answer open questions like what makes one senescent cancer cell different from another? Do senescent cells explain why some cancers relapse years after we thought they were cured?"
Dr Goel is confident that this work will lead to the discovery of some of the first ‘senotherapies’ – medicines that specifically target senescent cells.
Each of these researchers are being supported in their ambitious endeavours by eight-year Snow Fellowships of $8 million each, awarded by the Snow Medical Research Foundation thanks to the generous support of Terry and Ginette Snow and family.
The Fellowships are the biggest philanthropic investment in emerging biomedical research leaders in Australia, and crucially will allow each of these outstanding young researchers to focus on their research in a strategic way not otherwise possible in Australia.
“At Snow Medical, we want to back the boldest and best of the next generation of researchers. We set out to find exceptional visionary leaders, and our 2021 Snow Fellows are truly outstanding,” Snow Medical Chair Tom Snow said.



 Australia; NSW; VIC
Australia; NSW; VIC