News release
From:
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Jaya Dantas is Professor of International Health in the School of Population Health at Curtin University
Two years since the start of COVID-19 in late 2019, the pandemic is still all around us and we have had significant outbreaks and waves in all Australian states. There are millions of people with a compromised immune systems (those undergoing cancer and stem cell treatments, with conditions like rheumatoid arthritis, lupus, and other auto-immune diseases, transplant patients and others with severe chronic conditions). A significant proportion of the immunocompromised don't respond to COVID-19 vaccines, so despite being vaccinated, they are unsure if they are protected or not. This priority group is also at a higher risk of other infections, and COVID-19 was a significant threat that impacted their lives.
It will give immense hope to this group and those who could not be vaccinated due to medical conditions that can cause adverse reactions to vaccines, to learn that as of 24 February 2022, the TGA has provisionally approved the use of Evusheld, which is a long-acting monoclonal antibody combination of (150mg of tixagevimab co-packaged with 150mg of cilgavimab).
Evusheld is to be used as a pre-exposure prophylaxis (prevention measure) of COVID-19 in immune-compromised populations and those with medical conditions and cannot be vaccinated aged 12 years and over and weighing 40 kilograms or more.
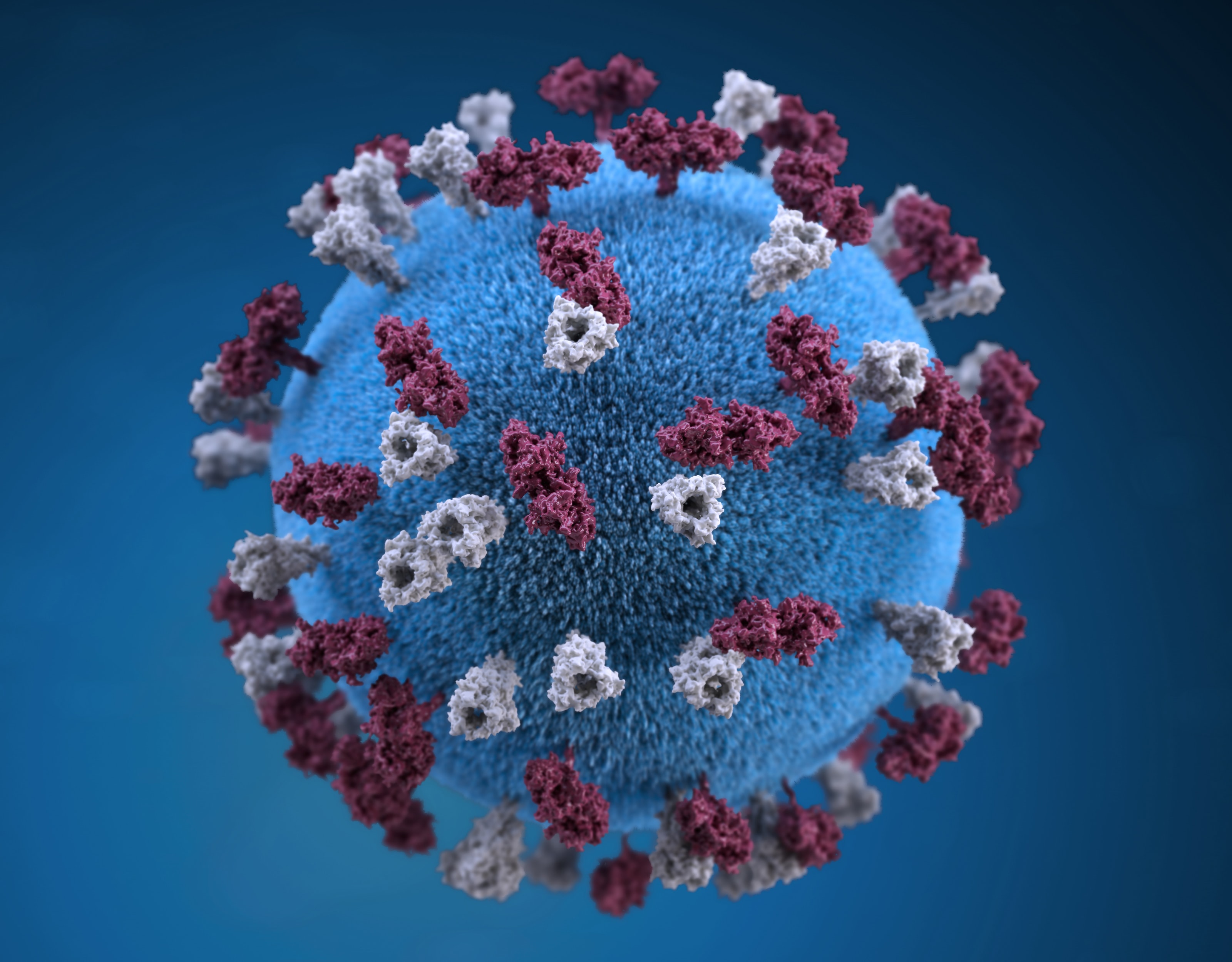
During Phase III trials, it was found that by combining two antibodies that have different and complementary activities against the virus, Evusheld had potential resistance to the emergence of new SARS-CoV-2 variants. These antibodies bind the spike protein of the SARS-CoV-2 virus at two different sites and stop the virus from entering the body and causing infection in human cells. Trials have shown Evusheld to be effective for six months and it is administered as two separate, sequential liquid injections of the two long-acting antibodies, tixagevimab and cilgavimab injected into the muscle by a doctor or a nurse. Currently, 36,000 treatment doses of Evusheld have been ordered by the Federal Government and use will be strictly monitored for safety, efficacy and adverse reactions.
Cassandra Berry, is a Professor in Viral Immunology at Murdoch University.
Pre-exposure prophylaxis is a preventative treatment usually given to people of high risk of disease when exposed to virus such as those who are immunocompromised or immunosuppressed.
In this case, two types of monoclonal antibodies (pre-made synthetic antibodies against the spike viral protein) are administered to individuals ahead of potential exposure or soon after infection with the virus. They will bind and block the virus from entering the body’s cells and significantly reduce the risk of developing symptomatic COVID-19.
This is a form of passive immunity rather than active immunity.
Pre-exposure prophylaxis with these antibodies is only effective for about six months and does not last forever. So, it is a complimentary protective measure for COVID and is not a substitute for vaccination, which does induces immune memory.
Professor Paul Griffin is the Director of Infectious Diseases at Mater Health Services and the Head of the Mater Clinical Unit for the University of Queensland School of Medicine
We are very fortunate to have an array of now not only safe and effective vaccines but also therapies to combat COVID-19. Unfortunately, however there is a proportion of our population through their immune systems being unable to respond inherently or as a result of therapies to treat autoimmune, inflammatory or malignant conditions or prevent rejection of transplanted organs, that are unable to respond sufficiently to receive the same levels of protection that most of us derive from being vaccinated.
Due to these same conditions that reduce the response to vaccination, these individuals are often also at risk of more severe disease as a result of COVID-19.
Evusheld is a combination of two antibodies (tixagevimab and cilgavimab) that is given in a way that’s quite similar to vaccination in that it is injected into a muscle, however the two antibodies are given separately, so it's two injections. These antibodies can bind the spike protein on the virus in two different sites so work well together to give recipients effective protection to reduce their chance of the virus entering the body’s cells and causing infection.
This effect is relatively long lasting, likely in excess of six months. As with all approvals, the TGA carefully considered clinical trial data which in this case included over 5000 participants and demonstrated that it was both safe and reduced risk of symptomatic COVID-19 by over 80 per cent. In my opinion this approval represents another significant step forward in our capability to control this virus and further limit its impact.



 Australia; QLD; WA
Australia; QLD; WA