News release
From:
Could a cancer drug hold the key to a HIV cure?
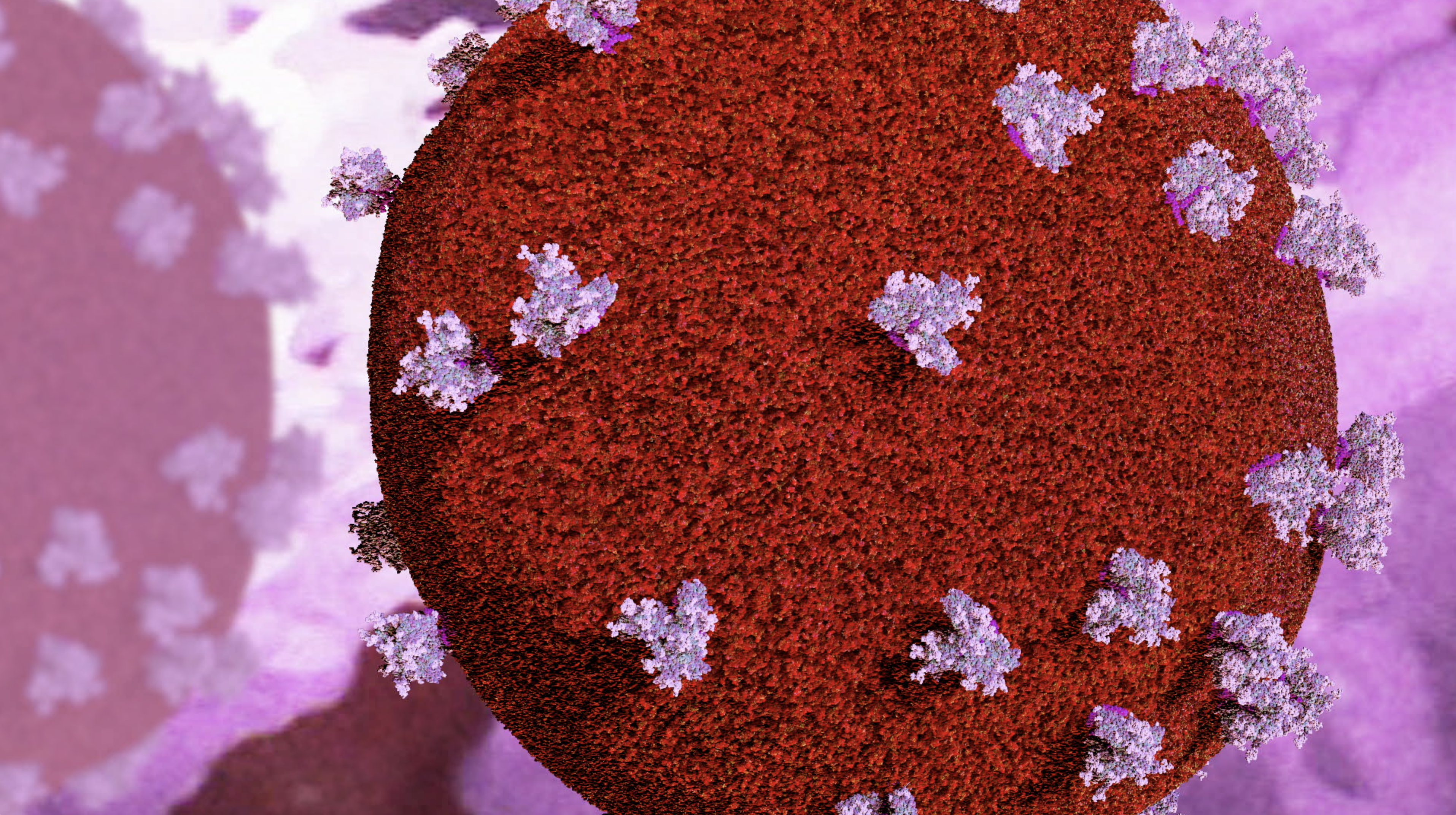
An existing blood cancer drug has shown promise in killing ‘silent’ HIV cells in animal models and human cells from people living with HIV – a significant pre-clinical discovery that could lead to a cure for the disease.
Hidden HIV cells, known as latent infection, are responsible for the virus permanently remaining in the body and cannot be treated by current therapy options. These hibernating, infected cells are the reason why people living with HIV require life-long treatment to suppress the virus.
Led by WEHI and The Peter Doherty Institute for Infection and Immunity (Doherty Institute), the landmark study is being translated into a new clinical trial to assess whether the blood cancer treatment can be repurposed to offer a pathway towards an HIV cure.
At a glance
- * A joint WEHI and Doherty Institute study finds the cancer drug venetoclax – based on a groundbreaking research discovery at WEHI – can kill hibernating HIV-infected cells and, crucially, delay the virus from re-emerging.
- * While current treatments can suppress the virus, they cannot target hibernating HIV-infected cells and permanently prevent the virus from coming back.
- * A clinical trial based on the findings will launch in Denmark and Australia, to test whether venetoclax can be used as a potential pathway to develop a cure for HIV.
An estimated 39 million people worldwide are living with HIV, including more than 29,400 Australians.
Antiretroviral therapy (ART) is the standard of care treatment given to people living with HIV and is highly effective. But the medication cannot target hibernating HIV-infected cells, meaning it can only suppress the virus – not cure it.
ART for people living with HIV is life-long: if a person stops taking this medication, hibernating HIV-infected cells will reactivate within a very short timeframe, leading to a resurgence of the virus. An estimated 98% of Australians living with HIV currently have undetectable levels of the virus, as it is completely suppressed by their ongoing ART treatment.
In the new study, WEHI researchers used the cancer drug venetoclax on enhanced pre-clinical models of HIV and found it delayed the virus from rebounding by two weeks, even without ART.
Co-first author, Dr Philip Arandjelovic from WEHI, said the discovery is an exciting step towards developing treatment options for the tens of millions of people currently living with HIV globally. “In attacking dormant HIV cells and delaying viral rebound, venetoclax has shown promise beyond that of currently approved treatments,” he said.
“Every achievement in delaying this virus from returning brings us closer to preventing the disease from re-emerging in people living with HIV. Our findings are hopefully a step towards this goal.”
The study marks the first time venetoclax has been used on its own to assess HIV persistence in pre-clinical models. However, researchers also found the cancer treatment can be combined with another drug that acts on the same pathway and is currently in clinical trials, to achieve a longer delay in viral rebound, with a shorter duration of venetoclax treatment.
“It has long been understood that one drug may not be enough to completely eliminate HIV. This finding has supported that theory, while uncovering venetoclax’s powerful potential as a weapon against HIV,” Dr Arandjelovic said.
Lifelong memory game HIV primarily targets CD4+ T cells, a type of white blood cell crucial for the immune system to properly function.
It is within these cells that HIV can lie dormant, ready to reactivate if the virus is not effectively eliminated. Using human CD4+ T cells donated by people living with HIV who are on suppressive ART, scientists at the Doherty Institute found venetoclax was also able to reduce the amount of HIV DNA in these white blood cells.
Co-first author, The University of Melbourne’s Dr Youry Kim and a Postdoctoral researcher at the Doherty Institute, said venetoclax potently reduced the amount of intact viral DNA in patient cells when studied in the laboratory.
“This indicates that venetoclax is selectively killing the infected cells, which rely on key proteins to survive. Venetoclax has the ability to antagonise one of the key survival proteins,” said Dr Kim.
Milestone trial
Venetoclax, marketed as VENCLEXTA, is based on a landmark discovery by Professor David Vaux AO in 1988. The drug is the result of a research collaboration between WEHI and companies Roche, Genentech (a member of the Roche Group) and AbbVie. It was developed by Roche, Genentech and AbbVie and co-developed and trialled in Australia. The Phase I/IIb clinical trial using venetoclax to treat HIV will start at the end of the year in Denmark, with plans to expand the study to Melbourne in 2024. It will be led by Professor Sharon Lewin (Director of the Doherty Institute), Professor Marc Pellegrini (Executive Director at the Centenary Institute) and Dr Thomas Rasmussen (clinician scientist at Denmark’s Aarhus University).
Prof Marc Pellegrini, a joint corresponding author and WEHI Honorary Fellow, said the trial will replicate the pre-clinical study conducted using WEHI’s state-of-the-art technology and facilities. “The trial will assess the safety and tolerability of venetoclax in people living with HIV who are on suppressive antiretroviral therapy,” said Prof Pellegrini, a former Head of WEHI’s Infectious Diseases and Immune Defence Division. Melbourne Laureate Professor Sharon Lewin, a joint corresponding author, concluded: “It’s exciting
to see venetoclax, which has already helped thousands of blood cancer patients, now being repurposed as a treatment that could also help change the lives of people living with HIV and put an end to the requirement for life-long medication.”
The research was supported by the National Health and Medical Research Council (NHMRC), The Sylvia & Charles Viertel Senior Medical Research Fellowship, Australian Centre for HIV and Hepatitis Virology Research, the Victorian Government and Australian Government.
The study, “Venetoclax, alone and in combination with the BH3-mimetic S63845, depletes HIV-1 latently infected cells and delays rebound in humanized mice”, involves collaborations with the University of Melbourne and Royal Melbourne Hospital, and is published in Cell Reports Medicine.
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Professor Anthony Kelleher is Director of the Kirby Institute, UNSW Sydney
The paper from Arandjelovic, Kim and co-authors shows that approaches previously used for the successful treatment of certain types of blood cancers increase the time to viral rebound in a humanised mouse model of HIV infection following anti-retroviral treatment interruption. While the effect is present using one drug, currently in routine clinical use, the effect is best observed using the first drug in combination with a second drug, which is in early phase development. The size of the effects, while statistically significant, are modest.
The goal of HIV cure or remission strategies is to prevent viral replication and progressive infection when a person living with HIV stops anti-retroviral therapy. To do this, the viral reservoir, which persists despite prolonged anti-retroviral therapy, must be eliminated or controlled. This reservoir exists in long-lived CD4+ T cells.
The authors used two drugs with similar modes of action, increasing cell death by apoptosis of lymphocytes, but each blocked different targets within the cell survival pathways. One drug, Venteoclax, is approved for the treatment of chronic lymphocytic leukemia, and the other, S63845, is undergoing assessment in early phase (phase 1) clinical trials for haematological malignancies. Venetoclax, alone and in combination with the BH3 mimetic S63845, depletes HIV-1 latently infected cells and delays rebound in humanised mice.
Venetoclax alone delays the time to viral rebound from 1 week to 2 weeks, while the 2-drug combination further delays the time to viral rebound to 3 weeks. Venetoclax, alone and in combination with the BH3 mimetic S63845, depletes HIV-1 latently infected cells and delays rebound in humanized mice.
These results suggest that this combination of drugs could be explored in helping to find a pathway to an HIV cure or prolonged remission. Although humanised mice are a standard model in which to study HIV therapeutics, results may not be transferrable to humans living with HIV, either in terms of efficacy or in terms of their side effect profile or toxicities, which can only be determined by systematic assessment through well designed human clinical trials. The authors are proposing to explore the safety and efficacy of the approach through clinical trials.
Multimedia





 Australia; NSW; VIC
Australia; NSW; VIC