News release
From:
Cancer: Cervical cells may aid the detection of ovarian and breast cancers
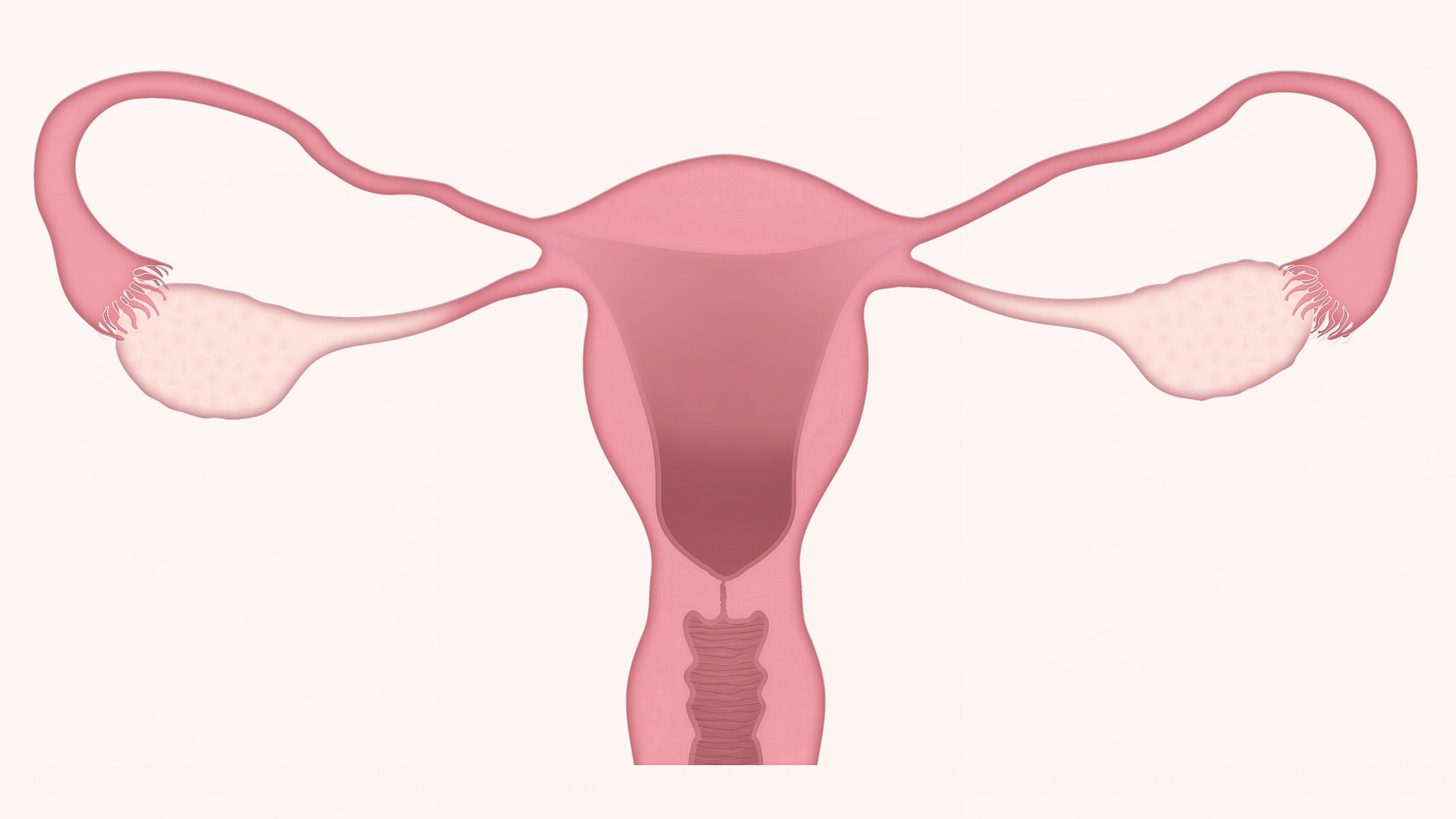
Cells collected during cervical cancer screening tests could be used to identify ovarian cancers, suggests a paper published in Nature Communications. A second paper reports the development of a test using cervical cells collected from routine screenings, which may be able to determine the presence of breast cancer. The findings, in small cohorts of women, may enable the earlier detection of both cancers.
Ovarian cancer is responsible for the largest proportion of deaths associated with gynaecological cancers. Currently, 75% of ovarian cancers are diagnosed at a late stage, when the tumours have spread, and being able to detect the disease earlier may improve treatment outcomes. Breast cancer is the most common cancer in females and is usually detected using mammography followed by a biopsy. Previous research has suggested that DNA changes could be used to predict the risk of developing these cancers.
Martin Widschwendter and colleagues used cervical cell samples collected from a cohort of 242 women with and 869 without ovarian cancer. The authors measured 14,000 epigenetic changes (molecular modifications that alter patterns of gene expression without the DNA itself being altered) in the screening samples. They identified a DNA methylation signature that could be used to identify or predict the presence of ovarian cancer. In the cohort, the methylation signature allowed the authors to identify 71.4% of women under 50 years of age and 54.5% of women over 50 years of age with ovarian cancers with 75% specificity. The findings were further validated in an additional cohort of women, where 47 had ovarian cancer and 227 did not, and found that women with higher scores may have an increased risk of ovarian cancer.
In a second study, the authors initially analysed epigenetic changes in cervical cell samples from 329 women with breast cancer with a poor prognosis and 869 women without breast cancer. They found they were able to identify women with breast cancer based on an epigenetic signature. They confirmed this finding in a smaller set of samples from 113 breast cancer patients and 225 women without breast cancer.
The authors indicate their findings suggest that using epigenetic signatures may aid in the detection of these cancers. However, the authors conclude that further research and large-scale prospective clinical trials are needed to determine whether these tests could predict the likelihood of woman developing either of these cancers.



 International
International