News release
From:
Peer-reviewed Experimental study Animals; Cells
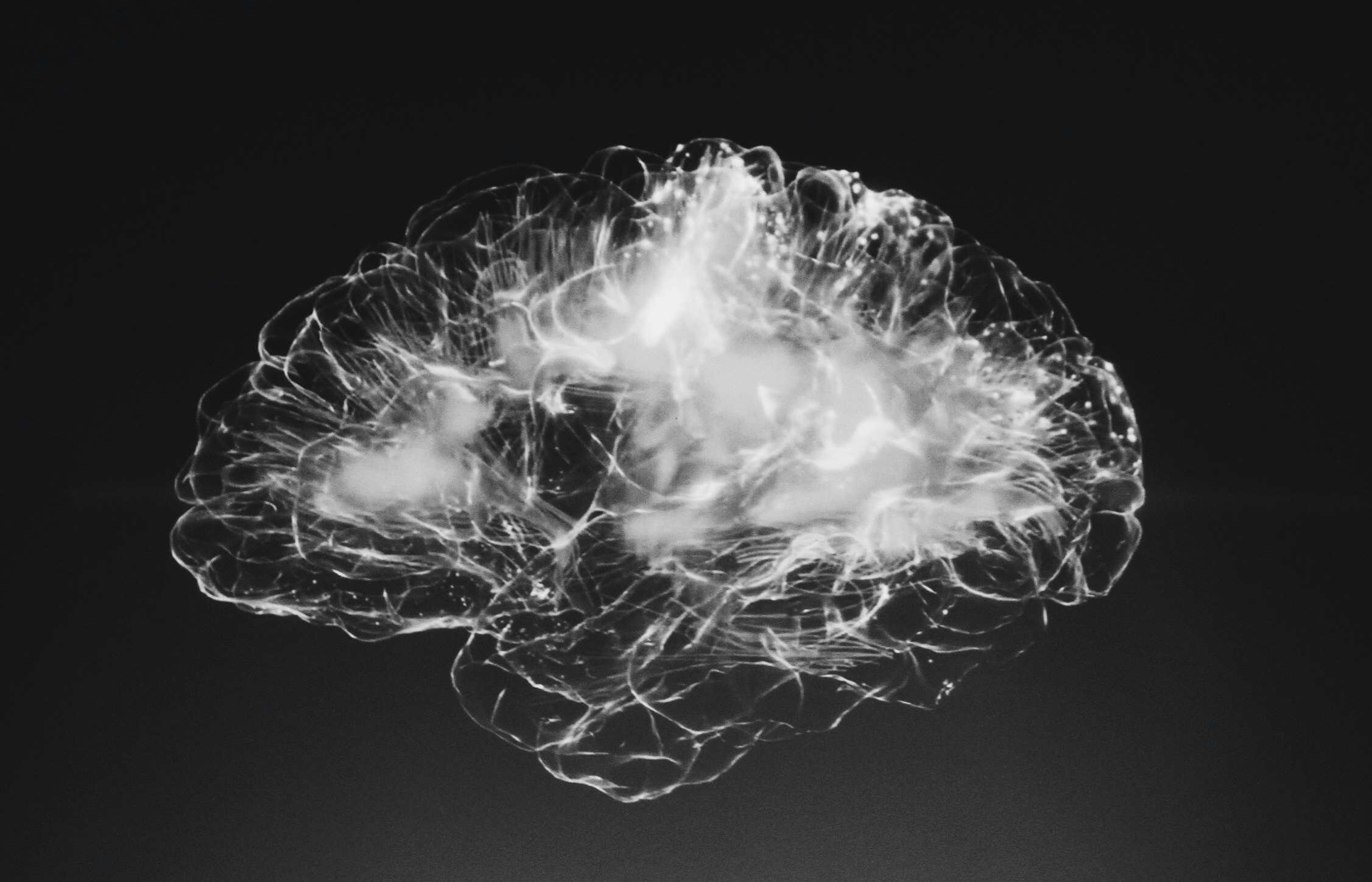
Brain’s support cells contribute to Alzheimer’s disease by producing toxic peptide
Targeting oligodendrocytes could help reduce amyloid beta production
Oligodendrocytes are an important source of amyloid beta (Aβ) and play a key role in promoting neuronal dysfunction in Alzheimer’s disease (AD), according to a study published July 23, 2024 in the open-access journal PLOS Biology by Rikesh Rajani and Marc Aurel Busche from the UK Dementia Research Institute at University College London, and colleagues.
AD is a devastating neurodegenerative disorder affecting millions of people worldwide. Accumulation of Aβ – peptides consisting of 36 to 43 amino acids – is an early critical hallmark of the disease. Recent clinical trials demonstrating a slowing of cognitive and functional decline in individuals with AD who are treated with anti-Aβ antibodies reinforce the important role of Aβ in the disease process. Despite the key cellular effects of Aβ and its essential role in AD, the traditional assumption that neurons are the primary source of toxic Aβ in the brain has remained untested.
In the study, Rajani and Busche showed that non-neuronal brain cells called oligodendrocytes produce Aβ. They further demonstrated that selectively suppressing Aβ production in oligodendrocytes in an AD mouse model is sufficient to rescue abnormal neuronal hyperactivity. The results provide evidence for a critical role of oligodendrocyte-derived Aβ for early neuronal dysfunction in AD. Collectively, the findings suggest that targeting oligodendrocyte Aβ production could be a promising therapeutic strategy for treating AD.
According to the authors, the functional rescue is remarkable given the relatively modest reduction in plaque load that results from blocking oligodendrocyte Aβ production, while blocking neuronal Aβ production leads to a near elimination of plaques – another hallmark of the disease. This small contribution of oligodendrocytes to plaque load could suggest that a main effect of oligodendrocyte-derived Aβ is to promote neuronal dysfunction.
Together with the data showing an increased number of Aβ-producing oligodendrocytes in deeper cortical layers of the brains of individuals with AD, these results indicate that oligodendrocyte-derived Aβ plays a pivotal role in the early impairment of neuronal circuits in AD, which has important implications for how the disease progresses and is treated. The increased number of oligodendrocytes in human AD brains also raises the intriguing possibility that these cells could potentially offset reduced Aβ production due to neuronal loss as the disease progresses.
The authors add, “Our study challenges the long-held belief that neurons are the exclusive source of amyloid beta in the brain, one of the key toxic proteins that builds up in Alzheimer's Disease. In fact, we show that oligodendrocytes, the myelinating cells of the central nervous system, can also produce significant amounts of amyloid beta which impairs neuronal function, and suggests that targeting these cells may be a promising new strategy to treat Alzheimer's Disease.”



 International
International