News release
From:
Immunology: Exploring the mechanism of vaccine-induced blood clotting
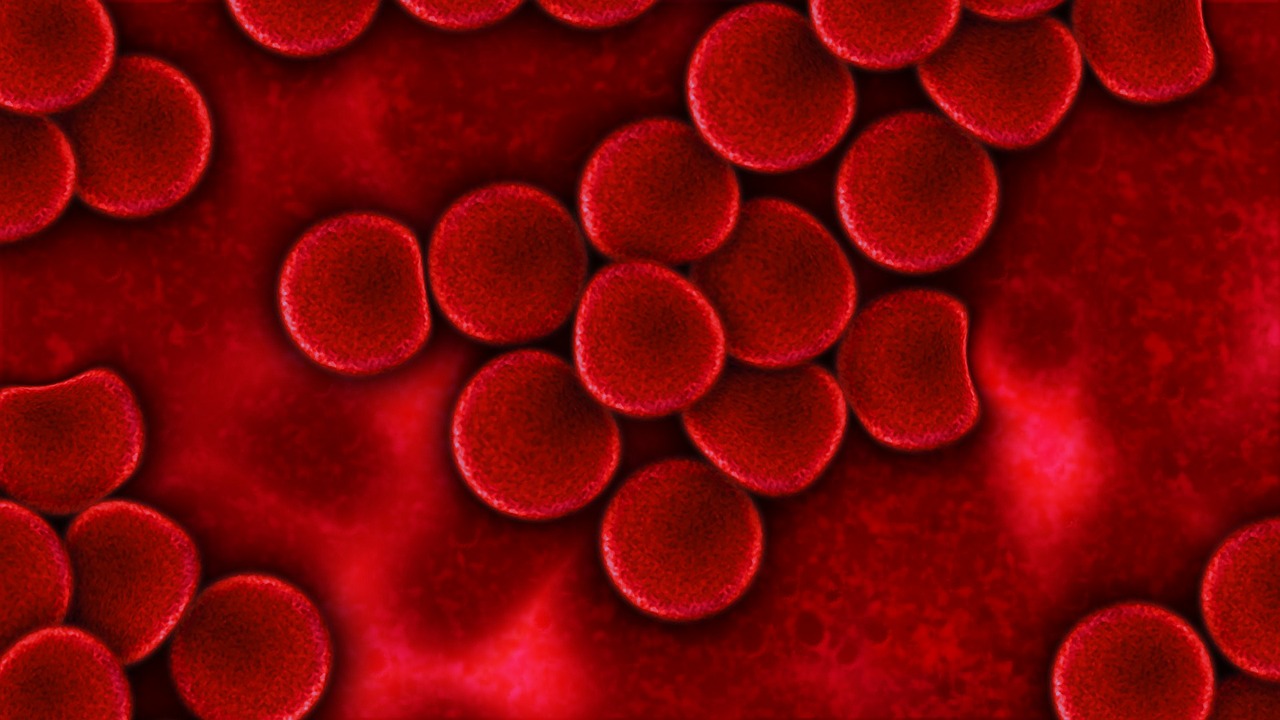
Insights into how some SARS-CoV-2 vaccine-induced antibodies may contribute to blood clotting seen in the rare condition vaccine-induced immune thrombotic thrombocytopenia (VITT) are provided in a paper published in Nature. The research finds that antibodies from five individuals with VITT, who had been vaccinated against SARS-CoV-2 with the AstraZeneca COVID-19 vaccine, bind to a protein involved in blood coagulation at the same point as the anticoagulant drug heparin.
VITT is a rare but serious adverse effect following administration of adenoviral vector vaccines against SARS-CoV-2 that results in low blood platelet counts (thrombocytopenia) and blood clots in the arteries or veins. VITT resembles heparin-induced thrombocytopenia (HIT) and previous research has shown that both are associated with the production of antibodies against a protein bound to platelets known as platelet factor 4 (PF4), which is involved in blood coagulation. However, the exact mechanism of how these antibodies cause VITT remains unclear.
Ishac Nazy and colleagues analysed serum from 5 patients with VITT (mean age of 44 years) who had received a single dose of the AstraZeneca vaccine. The authors found that antibodies obtained from the serum of these individuals and herapin bind to the same site on PF4. When compared to serum samples from 10 patients with HIT, they observed that the VITT antibodies had a stronger binding response to PF4. Nazy and co-authors suggest that the VITT antibodies bind to PF4 to form immune complexes; these in turn activate platelets via FcγRIIa receptors on their surface, which could initiate coagulation and cause thrombocytopenia and thrombosis. However, the authors note that this may not be the only factor that leads to the development of thrombotic events in patients with VITT and that other serum factors may be involved in platelet activation.



 International
International