News release
From:
Researchers from The University of Queensland have determined how Botox – a drug made from a deadly biological substance – enters brain cells.
Professor Frederic Meunier and Dr Merja Joensuu at UQ’s Queensland Brain Institute have discovered the specific molecular mechanism by which the highly deadly Botulinum neurotoxin type-A, more widely known as Botox, enters neurons.
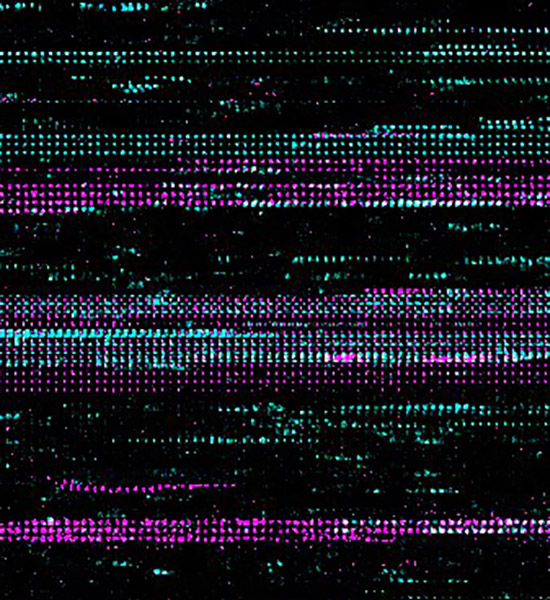
“We used super-resolution microscopy to show that a receptor called Synaptotagmin 1 binds to two other previously known clostridial neurotoxin receptors to form a tiny complex that sits on the plasma membrane of neurons,” Professor Meunier said.
“The toxin hijacks this complex and enters the synaptic vesicles which store neurotransmitters critical to communication between neurons.
“Botox then interrupts the communication between nerves and muscle cells, causing paralysis.”
The discovery means new therapeutic targets can be identified to develop effective treatments for botulism – a rare but potentially fatal bacterial infection.
“Now we know how this complex allows the toxin internalization, we can block interactions between any two of the three receptors to stop the deadly toxins from getting into neurons,” Professor Meunier said.
The injectable drug Botox was originally developed to treat people with the eye condition strabismus, but was quickly found to alleviate migraine, chronic pain, and spasticity disorders.
Now, it’s regularly used in plastic surgeries and is commonly known as a cosmetic treatment to smooth wrinkles.
Dr Joensuu said just how the neurotoxin worked to relax muscles has previously been difficult to track.
“Clostridial neurotoxins are among the most potent protein toxins known to humans,” Dr Joensuu said.
“We now have a full picture of how these toxins are internalised to intoxicate neurons at therapeutically relevant concentrations.”
UQ acknowledges the collaborative efforts of researchers from the Hannover Medical School, University of Edinburgh, and University of Helsinki.
This study was published in the EMBO Journal. (DOI: 10.15252/embj.2022112095)
Media: QBI Communications, communications@qbi.uq.edu.au, Merrett Pye +61 422 096 049.



 Australia; QLD
Australia; QLD