News release
From:
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Dr Rietie Venter is a Senior Lecturer and Head of Microbiology in the School of Pharmacy & Medical Sciences at The University of South Australia
Antimicrobial resistance (AMR) is a global threat that should be addressed with a global response. The commitment by Heads of State at the UN general assembly to adopt a broad, coordinated approach is therefore a much-needed and very timely global incentive. Good stewardship is needed; not only in the medical use of antimicrobials, but also in the use of antimicrobials in animal health, the abundant use of antimicrobials in agriculture and the widespread use of biocides in common household products as all these practices are hastening the development of AMR. To this extend, the banning of triclosan and 17 other chemicals in soaps by the FDA [in the USA] is an initiative that could be extended and adopted globally.
We grew up in the golden age of antibiotics. A world without effective antimicrobials – where a simple scratch could cost you your life and where most modern medical procedures would no longer be possible - is unthinkable. Yet, the development of new antimicrobials is not pursued by pharmaceutical companies due to the low profit margins. Therefore, funding to research and develop new antibiotics and to curb the development of resistance have to come from governments. The UN agreement is testimony to the commitment of nations to address AMR and prevent us from sliding into a post-antibiotic era.
The pledge is an acknowledgement from the world community that antibiotic resistance is a global issue and a catastrophe that is here now and we need to do everything we can to stop it in its tracks and possibly reverse it.
The issue is complex, requiring a multi-faceted approach involving governments, the scientific research community, the pharmaceutical industry, the medical community and, most importantly, the public.
Governments have a role to play in raising awareness about the issue but also to provide investment vehicles and incentives to the pharmaceutical industry to develop antibiotics, something we are seeing now in the US and Europe, which we need to replicate in Australia and elsewhere.
Scientific research is of utmost importance here and should be encouraged to deliver new treatment options and rapid diagnostic tools to distinguish between a bacterial infection and a viral infection for example, and if bacteria are resistant to certain antibiotics. These diagnostic tools should become available in every clinic and become a routine part of any antibiotic prescription.
Last but not least, public awareness campaigns to educate the public, for example about the improper use of antibiotics, are paramount to the success of this commitment. The pledge by the UN member states is a significant step in the right direction to address an issue that threatens modern medicine as we know it.
Liz Harry is Professor of Biology and Director of the ithree institute (infection, immunology and innovation) at the University of Technology, Sydney (UTS)
There are a range of diseases, not just infectious diseases, for which antibiotics are used routinely; in patients who are immunosuppressed - who have had chemotherapy or organ transplants - or after most routine operations. It doesn’t stop with humans - antibiotics are widely used in the agricultural sector.
Antimicrobial resistance (AMR) is an incredibly serious issue and the solution isn’t simple. The UN declaration provides a much-needed standpoint from which all countries can coordinate development of action plans. Last year in Australia, the Commission on Safety and Quality in Health Care released its first national antimicrobial resistance strategy. It has since developed national surveillance surveys of AMR and antibiotic use in human health, animal health and agricultural settings. This is an important first step in getting a handle on the scale and severity of the issue.
Almost all the microbes we coexist with are essential for good health and they sustain our environment. At the i3 institute we focus on understanding how microbial communities harmoniously live and thrive; and imbalance leads to infectious disease. But it is not just about developing new antibiotics. We can now use technology to determine what underpins a stable microbial ecosystem and find other tools and mechanisms to moderate and maintain this balance.
In addition to the usual players, from governments to industry and health professionals, the community has the right and the power to bring about change. This requires clear and consistent messaging of what AMR is and the delayed consequences of choosing medications and home disinfectants, such as triclosan, that cause bacteria to evolve and adapt - rendering these approaches useless in times of need.
This is a problem that is not too late to tackle. The stop smoking campaign is a great analogy that can be applied to reducing the antimicrobial resistance crisis.
Michael Gillings is Professor of Molecular Evolution in the Department of Biological Sciences at Macquarie University
Antibiotics were one of the greatest discoveries of the 20th Century. They have saved countless lives, including mine, and probably yours.
However, antibiotics are now becoming much less effective as more and more bacteria become resistant. We face a bleak future, where a simple wound or infection could kill. It is estimated that resistant infections will kill 10 million people per year by 2050, more than cancer. We need to protect the antibiotics we still have, we need to use alternative methods for disease control, and we need to develop new antimicrobial compounds.
These efforts require international cooperation. Like many issues that face humanity, antibiotic resistance is a global problem that requires global solutions.
Dr Taghrid Istivan is Senior Lecturer in Microbiology at RMIT University
What's the scale of the antimicrobial resistance problem?
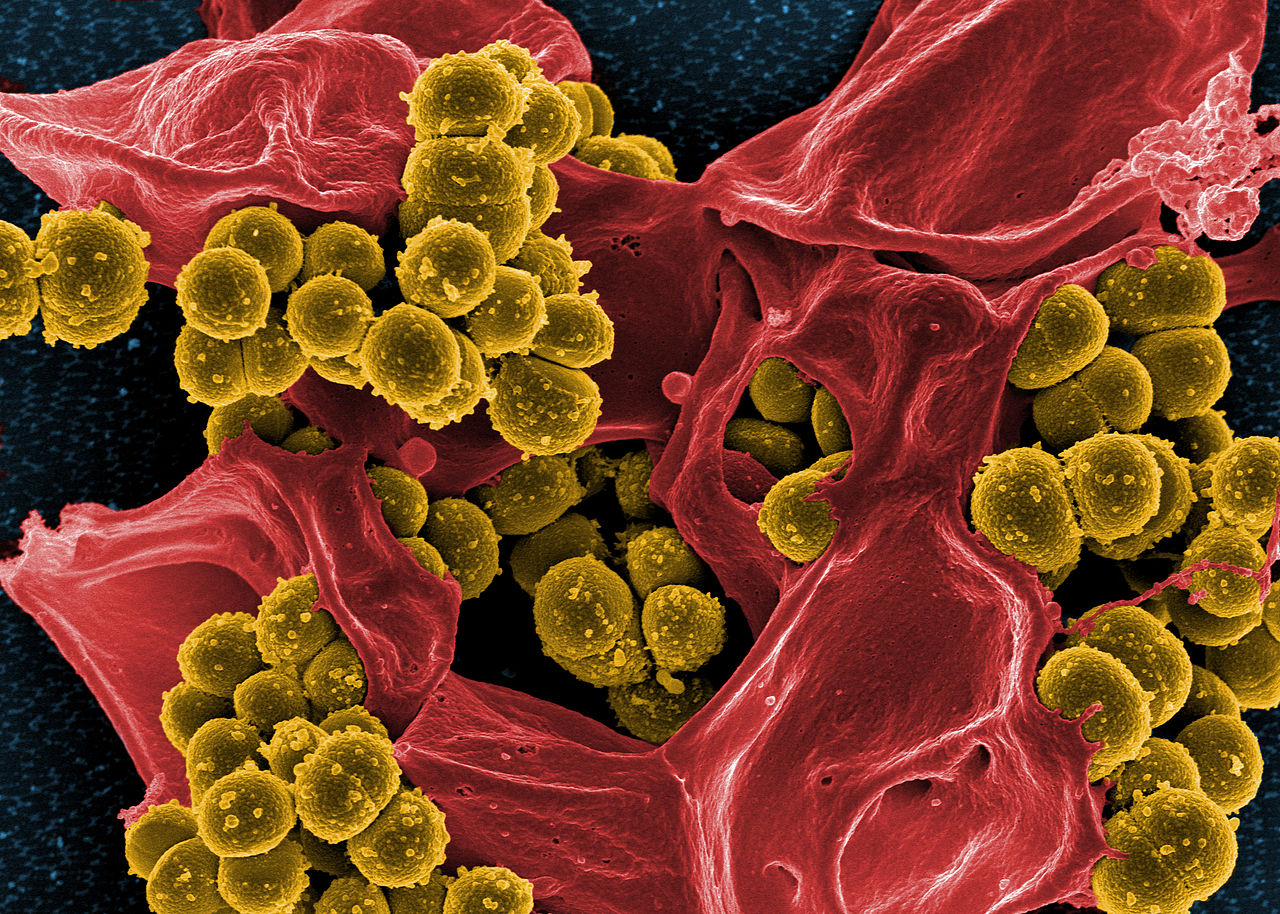
"Antimicrobial resistance is a global, world-wide problem which is increasing in both developed and developing countries leading to serious consequences in public health. Resistance to antimicrobial drugs has increased all over the world due to the uncontrolled use (overuse and misuse) of these drugs in human medicine, in food animals and in agriculture to prevent infections and improve productivity. The lack of controls and measures on antibiotics use in some countries has led to the emergence of multi-resistant microbes which can spread globally through travellers and food products. Microbes which are resistant to a broad range of antimicrobial drugs (normally called superbugs) are sometimes impossible to treat, leading to a high mortality rate, mainly in developing countries."
What are the reasons for the problem?
"Antibiotic resistance is a genetic property in microbes which is contained in the DNA and transferred to the offspring (inherited). Furthermore, some antimicrobial resistance characters (genes) in bacteria can be found on small mobile (transferable) pieces of DNA (plasmids) which are acquired and shared by different species (groups), existing in the same environment, as a response to prolonged antibiotic pressure, as a survival mechanism. This is behind the emergence of antibiotic resistance in microbes which were known to be susceptible to these antibiotics in the past. It is also leading to multi-resistance to antibiotics where more than one type of plasmid can be acquired by a bacterial cell."
The WHO Global Action Plan on Antimicrobial Resistance – what does it say?
"A global action plan by the World Health Organization is a critical approach to face antibiotic resistance. This could be effective if all countries adopt these measures and act towards achieving them. The main objectives in this WHO plan are:
- Public awareness and understanding of antimicrobial resistance through effective communication, education and training.
- Strong knowledge and evidence base surveillance and research.
- Through effective sanitation, hygiene and infection prevention measures to reduce infection.
Optimising the use of antimicrobial medicines in human and animal health and the development of sustainable investment that takes account of the needs of all countries, and very importantly to increase investment in new medicines, diagnostic tools, vaccines and other interventions."
Associate Professor Sanjaya Senanayake is a specialist in Infectious Diseases and Associate Professor of Medicine at The Australian National University
It is reassuring to hear the UN member states have made a pledge to make a coordinated global response to combat antibiotic resistance.
It was also important to see a non-medical figure and leading international diplomat such as Ban Ki-Moon talking about the deaths of 200,000 newborns every year due to antibiotic-resistant infections, and a host of antibiotic-resistant infections, such as typhoid, gonorrhoea, HIV/AIDS and TB. This shows that the world's political leaders are officially acknowledging on the global stage that this is a problem.
But the goodwill coming out of today's meeting must be followed up by the less exciting but nevertheless vital documented/signed commitment to funding, surveillance, research etc. Otherwise the momentum from today's meeting will be lost and the problem of antibiotic resistance will continue to grow.
Antibiotic resistance is responsible for 700,000 deaths globally and 50,000 deaths within the USA and Europe every year. By 2050, if the problem is not addressed, it will potentially cause ten million deaths per year at a cost of $100 trillion dollars.
What is most worrying is that this is already happening now, and only within 80 years of antibiotics being used. It doesn’t simply involve the medical sector, but also the pharmaceutical, agricultural and farming industries. Due to its complexity and enormous reach, global political will is needed to address and fund this problem. The political recognition is now there with official reports and bodies created by the Obama and UK governments to tackle antibiotic resistance.
However, today’s historic meeting of the UN General Assembly (only the 4th for an infectious diseases issue) will take this problem to another level, giving its profile a massive boost with all 193 member nations hopefully becoming signatories to combat this problem.
While this unprecedented recognition of antibiotic resistance is good, it would be ideal if firm targets were proposed at the UN, such as per capita antibiotic consumption, and firm commitments to funding. One scientist involved in the panel today’s meeting has previously suggested $5 billion/year.
If there is a lack of universal commitments from today’s UN meeting from all the member states, especially with regard to funding, it will be disappointing, despite the high profile it brings to this issue.
Decisive coordinated global action and funding is required now.
Professor Mary-Louise McLaws is a Professor Epidemiology of Hospital Infection and Infectious Diseases Control at the University of New South Wales
Preventing Antibiotic resistance from becoming an even bigger pandemic requires us all to act responsibly; when we attend our general practice with a respiratory tract infection we need to be mindful that most of the time we may have a virus that won't respond to antibiotics and in fact antibiotic treatment for viruses can place bacteria in our body, that are not causing us any problem, under pressure to develop resistance.
Your doctor may want you to wait a few days as we mostly improve after three days of feeling miserable. But take your doctor's advice and return for another consultation if your cold- or flu-like illness doesn't improve. It's a wake-up call that antibiotic use in the community peaks in flu season and causes a peak in antibiotic resistant diarrhoea. We excrete the antibiotic we consume into the sewerage system and we haven't researched the flow-on effect to the environment.
Doctors prescribing antibiotics in public hospitals have been audited and found that a quarter have been given inappropriately. Doctors must be mindful and prescribe according to our excellent Australian guidelines and in accordance with the hospital's Antimicrobial stewardship program. Patients can ask their doctor in hospitals and GP what they are being given and why they are being given an antibiotic, and take their treatment according to advice.
Hospital cleaning is more important than we credited it. It's pivotal for removing bacteria that include antibiotic resistant bacteria from the patient environment. All healthcare workers must not touch you without using alcohol-based hand rub as this is one of the most effective methods of reducing the spread of an infection that requires antibiotic treatment. And finally, we must demand our food animals to be antibiotic-free so we don't consume unnecessary antibiotics that could place our own bacteria under stress to produce resistance.
Antibiotics are a treasure and we all need to protect them for our future by reducing unnecessary use and healthcare workers must practice hand hygiene to prevent infection transmission as these will inevitably need antibiotic treatment.



 Australia; International
Australia; International