Media release
From:
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Professor David Murdoch is Dean and Head of Campus, University of Otago, Christchurch and Co-Director of One Health Aotearoa
Collection of the best possible sample is a critical for any diagnostic test. A test result can be misleading if the sample tested has not been collected in the right manner or is of the wrong type.
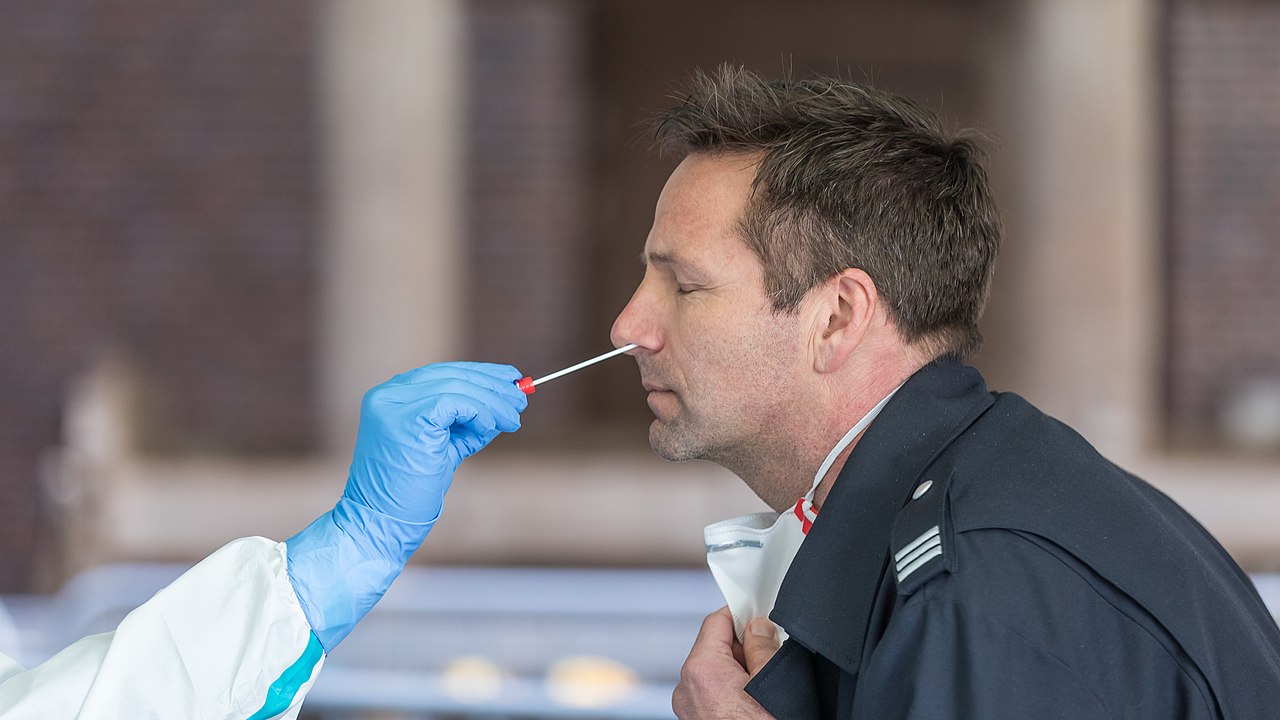
This study evaluated whether testing saliva might be a suitable alternative to the usual method of testing swabs from the back of the nose (nasopharynx). The saliva samples were collected by asking patients to repeatedly spit into a sterile urine cup until roughly a third full of liquid. The results of the study indicated that saliva performed as well as nasopharyngeal swabs at detecting cases of COVID-19, and indeed performed slightly better.
These findings are important because saliva samples can be obtained relatively easily and can be collected by the patient themselves without the need for swabs. The authors offer a word of caution in noting that their study only included patients who had moderate or severe disease and that the findings may be different when testing people with mild or asymptomatic disease. They also only collected samples first thing in the morning. So, it will be important to evaluate the performance of saliva samples in people with mild disease and in specimens collected at other times of the day as well in order to gain more confidence in these promising findings.
Dr Nikki Freed is a Senior Lecturer in the School of Natural and Computational Sciences at Massey University
This study is very promising. While still preliminary and not yet peer-reviewed, the work shows that saliva may be better than nasopharyngeal swabs for testing for the virus that causes COVID-19. The authors show that saliva had better sensitivity and was more consistent for detection of the virus than nasopharyngeal swabs.
From my perspective, saliva has a lot of advantages over nasopharyngeal swabbing, namely that it is easy to self administer and non-invasive. Most people can easily spit in a cup! Nasopharyngeal swabs, on the other hand, require a health care worker to get fully dressed in PPE and can be uncomfortable for the patient. So this study is a win-win.
This is one of the first studies to clearly show the clear advantages from the sensitivity and consistency aspect of using saliva instead of nasopharyngeal swabs.
Alternative COVID-19 testing samples to the current nasopharyngeal swabs used potentially relieve pressure on swab supplies and also allow the use of patients collecting their own samples (avoiding potential exposure to front-line testing staff taking swabs).
This study by New Zealander Dr Anne Wyllie at Yale School of Public Health indicates that the levels of COVID-19 virus were higher in the saliva samples than the transport media the swab is mixed in. However it should be noted that levels of virus are traditionally ‘diluted’ by mixing the swabs in a relatively large volume of transport media. Therefore a comparison of direct testing of swabs vs saliva would be of strong interest.
Other tests have been validated using saliva (Rutger University) and therefore the use of saliva as an alternative to swabs is of high interest to COVID-19 testing strategies




 New Zealand; International
New Zealand; International