News release
From:
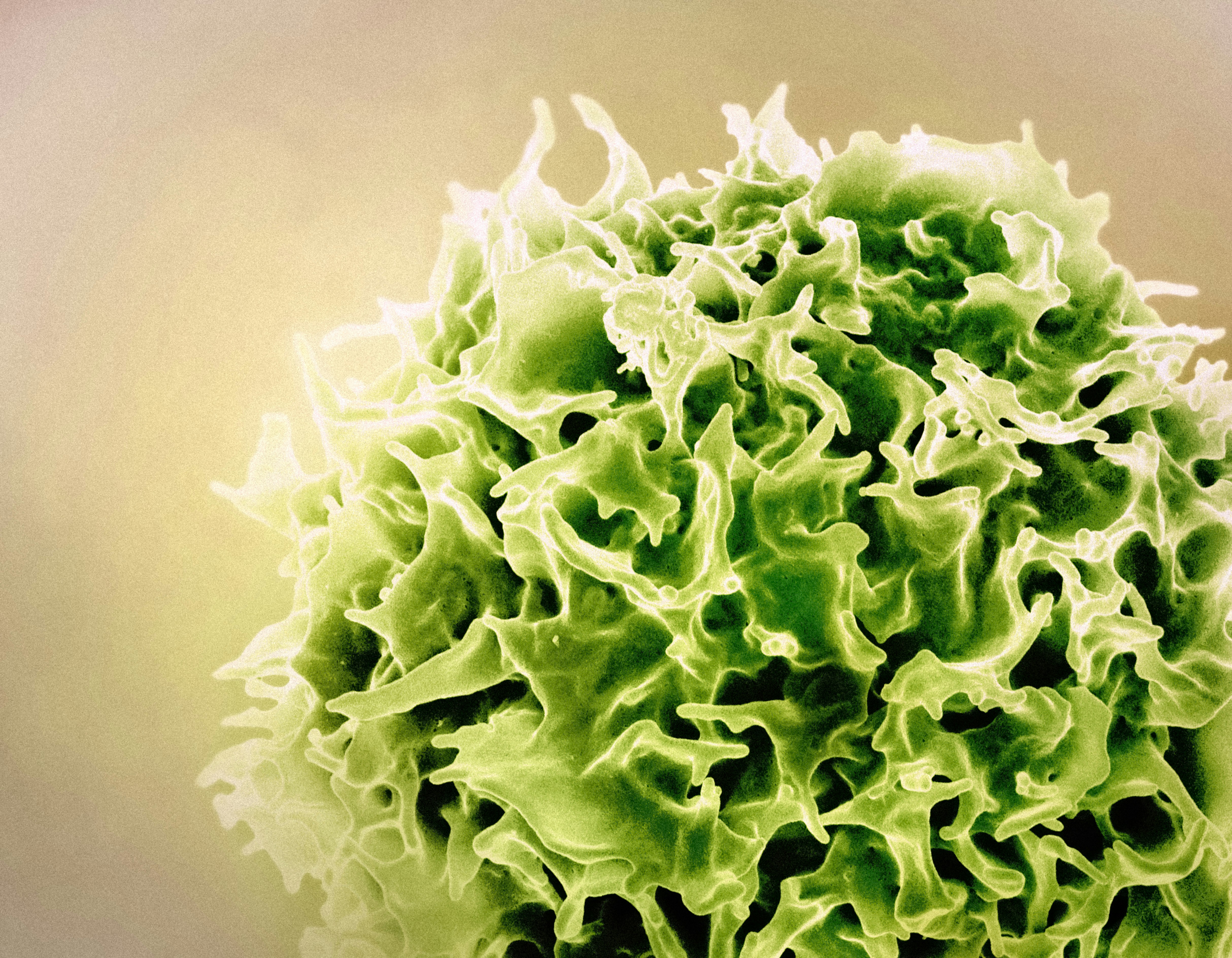
Rallying more T-cells to immunotherapy’s fight against cancer
Australian scientists have found a way to improve the effectiveness of cancer-fighting T cells within tumours, a potential step towards enabling more patients to respond to a life-saving immunotherapy.
Immune Checkpoint Blockade (ICB) has revolutionised the treatment of cancers like melanoma, but up to 60% of patients don’t respond to this immunotherapy for reasons not yet fully understood.
A collaborative study led by professors Phil Darcy and Paul Beavis from Peter Mac, and Associate Professor Jason Waithman from The University of Western Australia, has identified a new way to enhance the quality and durability of anti-tumour T cell responses, findings that could potentially enable ICB to work for more patients in the future.
Results of this research have just been published in the journal Nature Immunology.
“We know one of the ways cancer hides from our immune system is by silencing T cells, and ICB works by blocking receptors on these T cells so the cancer can no longer switch them off,” explains Professor Darcy who is Group Leader of Peter Mac’s Cancer Immunotherapy laboratory.
“Our research has identified a new way to ensure better-quality, long-lived T cells are generated and maintained so that when they reach the tumour tissue, ICB can keep them engaged in the fight against cancer.”
The process involves a protein called Fms-related tyrosine kinase 3 ligand (Flt3L) which occurs naturally in the body and which is required for healthy functioning of dendritic cells - key immune cells which instruct T cells how and when to respond.
The researchers demonstrated that increasing Flt3L levels expanded specialised dendritic cells in the lymph node closest to the tumour - where the immune response starts - which in turn primed a population of early-phase T cells capable of sustaining anti-tumour responses.
An enhanced tumour killing effect was observed in mice treated with lab-generated Flt3L and an ICB drug (anti-CTLA-4 therapy).
“We feel understanding this pathway, and the involvement of Flt3L, is key to improving response rates to this potent immunotherapy,” Prof Beavis says.
Co-first authors of this paper include Dr Junyun Lai and Cheok Weng Chan (Peter Mac) and Dr Jesse Armitage (Peter Mac & The University of Western Australia).
This work was funded via various National Health and Medical Research Council (NHMRC) grants, and supporters also included the New York-based Cancer Research Institute.
The paper is titled “Flt3L-mediated tumor cDC1 expansion enhances immunotherapy by priming stem-like CD8+ T cells in lymph nodes”.
About Peter Mac
Peter MacCallum Cancer Centre is a world leading cancer research, education and treatment centre and Australia’s only public health service dedicated to caring for people affected by cancer.



 Australia; VIC; WA
Australia; VIC; WA