Media release
From:
NEWS BRIEFING: Revolutionary blood cancer treatment CAR T-cell therapy shows first signs of fighting solid tumours too
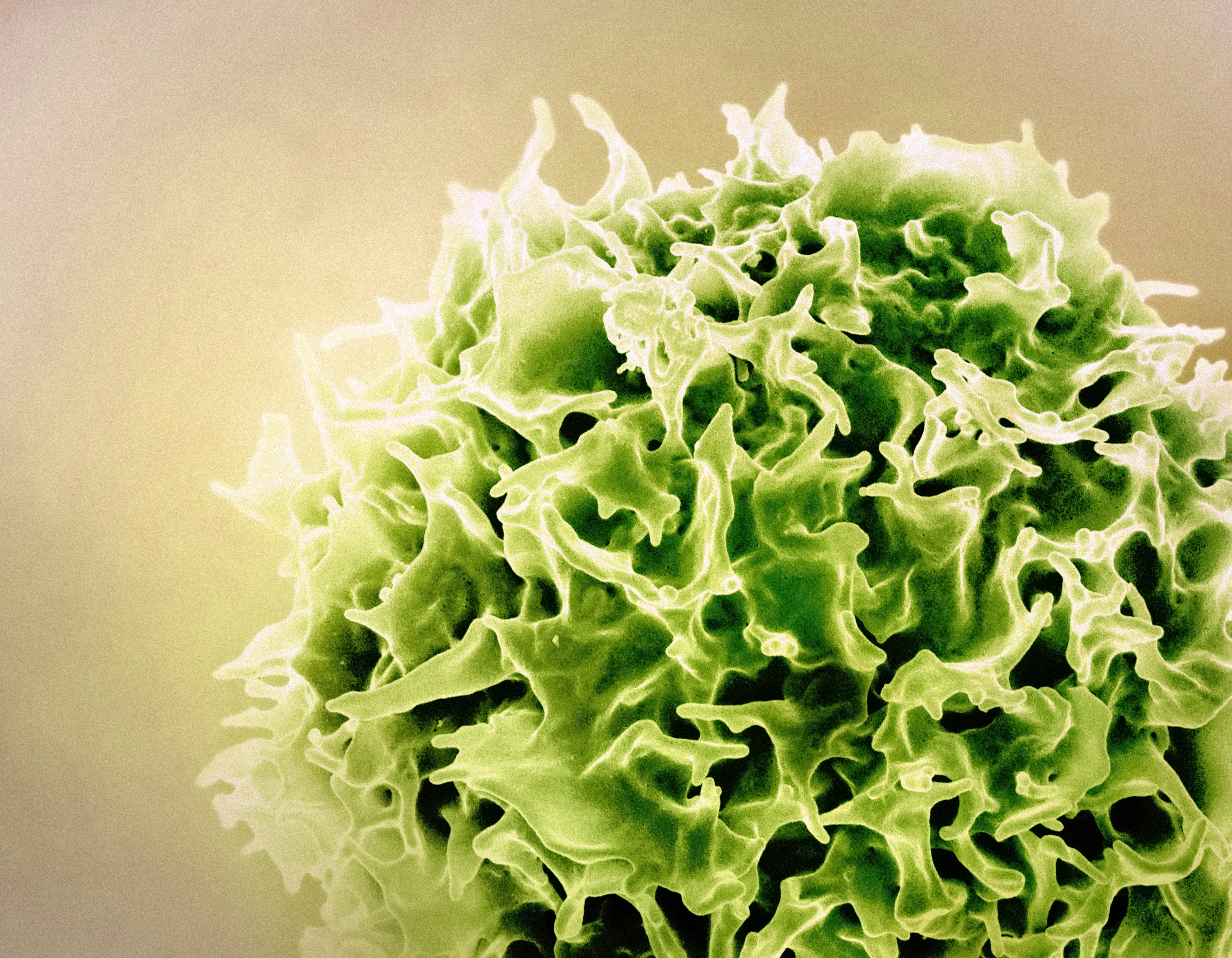
Chimeric Antigen Receptor (CAR) T-cell therapy is an emerging immunotherapy which can cure patients with aggressive blood cancers who have exhausted all other treatment options. But it has not proven effective against solid tumours, which account for 90% of all cancers, until now.
In new research led by Peter Mac scientists, gene editing techniques were used to 'armour' CAR T-cells to produce additional proteins, enabling them to target cancer cells in solid tumours successfully. The team says their tests suggest these modified CAR T-cells have the potential to treat many common types of cancer, including breast, colon and ovarian cancer. Cure rates in their tests on mice with solid tumours were close to 100%.
The researchers have overcome two major hurdles preventing CAR T-cells from being an effective treatment for solid tumours. Previously, armoured CAR T-cells damaged healthy body cells as well as tumour cells. Targeting them to attack cells in tumours also proved tricky because - unlike blood cancer cells – cells in solid tumours lack uniformity, meaning there is no common target.
The team overcame these issues by identifying two areas of DNA that were activated in CAR T-cells once inside a tumour. They used these to program the CAR T-cells to release anti-cancer proteins, called cytokines, only inside the tumour. This is a critical first step to enabling CAR T-cell therapy to revolutionise treatment of solid cancers, as it has for blood cancer.
Join us for this online briefing to hear from the Peter Mac experts behind the research.
Speakers:
- Associate Professor Paul Beavis is Co-Head of the Cancer Immunology Program at the Peter MacCallum Cancer Centre
- Professor Phil Darcy is Co-Head of the Cancer Immunology Program at the Peter MacCallum Cancer Centre
Date: Wed 02 July 2025
Start Time: 10:00 AEST
Duration: Approx 45 min
Venue: Online - Zoom
Briefings are free to attend, but if you like what we do, you can donate to the Australian Science Media Centre here



 Australia; VIC; WA
Australia; VIC; WA