Media release
From:
Drug which stops tumors' blood supply could help kids with bone cancer live longer
Children with multi-metastatic Ewing’s sarcoma face very poor survival rates — now an early trial of pazopanib shows promise for helping them live longer, healthier lives
Survival rates for children with multi-metastatic Ewing’s sarcoma — a kind of bone cancer which has spread to multiple parts of the body — are ‘dismal’, scientists say. The five-year survival rate for children with this cancer is very low — some studies suggest less than a quarter reach this milestone. But a small non-randomized retrospective study of a drug called pazopanib has shown that it increases children’s survival without major side-effects. 85% of patients taking the drug survived for two years after diagnosis, and two-thirds reached the end of the second year without their cancer progressing. Researchers urge the development of larger-scale trials to investigate further.
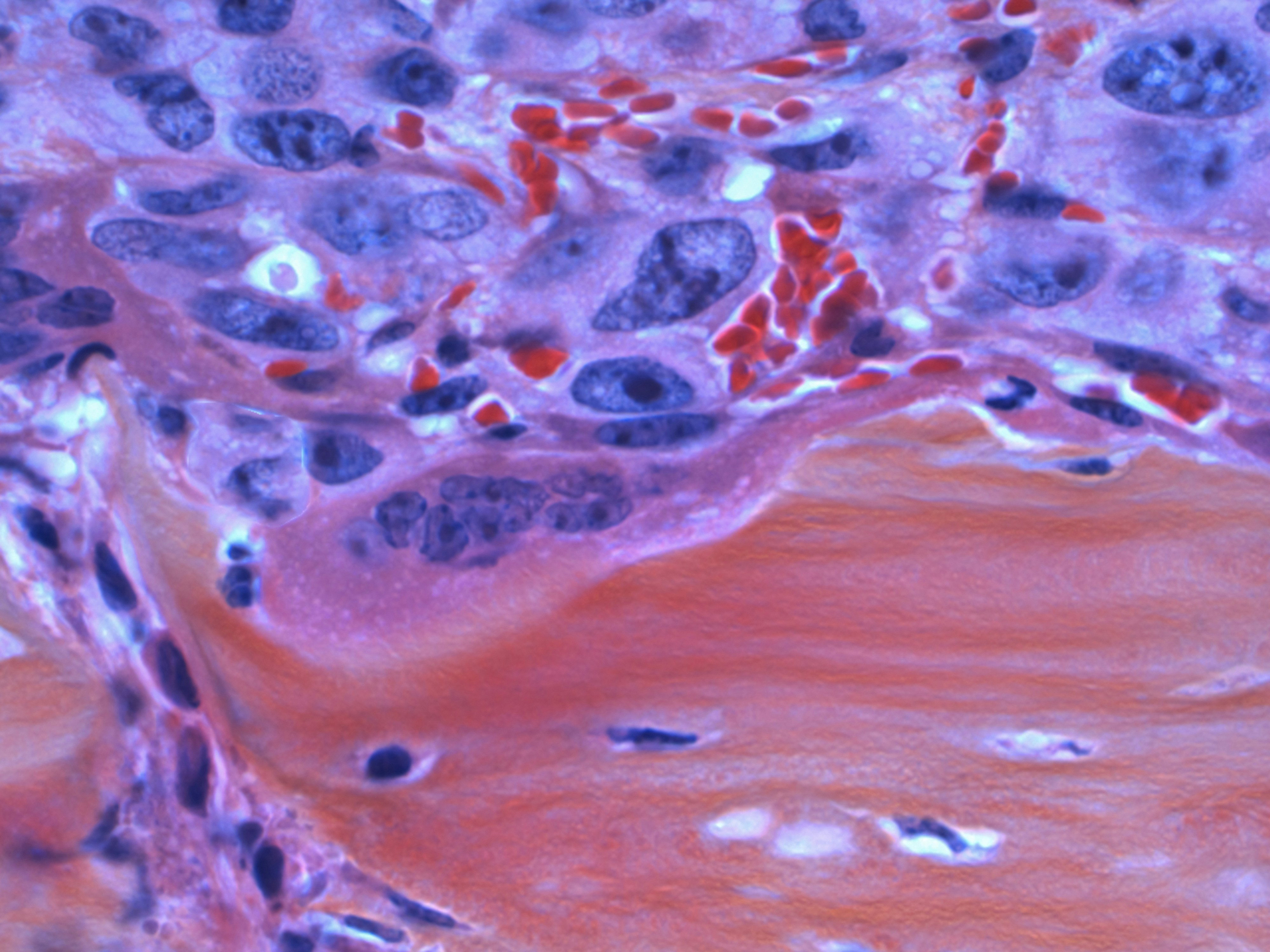
Ewing sarcoma is one of the most common bone cancers seen in children, and if it spreads, it can be deadly. One study found that under a quarter of children with multi-metastatic Ewing sarcoma survived five years after their diagnosis. Now scientists have found that a drug called pazopanib had striking success in treating a small group of young patients. 85% of their patients survived two years after diagnosis, and two-thirds saw no disease progression. The team calls for larger studies which can develop this treatment further.
“Survival rates were higher than in historical controls, suggesting it may extend lives and, importantly, do so without adding severe toxicity,” said Prof Anna Raciborska of the Warsaw Mother and Child Institute, lead author of the article in Frontiers in Oncology. “Moreover, the quality of life of treated children was good. After the end of IV treatment, patients could receive pazopanib as a home treatment.”
“While we wait for new treatment options, it is possible to implement this existing drug to improve outcomes in very high-risk patients,” she added. “It opens the door to targeted therapies earlier in the disease course, potentially improving survival and quality of life.”
A potential lifesaver
Pazopanib was originally developed for renal cell carcinoma. But after some success in adult patients with Ewing sarcoma, Raciborska and her team tried incorporating it into the treatment regimens of child patients with multi-metastatic Ewing sarcoma, in the hope that combining it with other treatments would produce a better result by targeting different aspects of the cancer simultaneously.
“Pazopanib is a pill that blocks the tumor's ability to grow new blood vessels, which tumors need to survive and spread,” said Raciborska. “By cutting off this ‘blood supply’, the drug presumably makes tumors weaker and more sensitive to chemotherapy and radiation. This may slow down the disease and help existing treatments work better.”
Between 2016 and 2024, 11 young patients were given pazopanib alongside standard first-line treatments at the Warsaw Mother and Child Institute. The success of this additional treatment was tracked as part of their regular care, with imaging and lab tests, and careful monitoring of any possible side-effects. The goal was to determine whether the additional treatment helped control their cancer, and whether any side-effects were manageable.
A glimmer of hope
The 11 patients ranged in age from five to 17 when they started taking pazopanib. They took pazopanib during and after their chemotherapy, although treatment was paused for surgery and stopped if the disease progressed or patients experienced unacceptable side effects. On average, the patients took pazopanib for 1.7 years. At the time of writing, six were still taking pazopanib.
Five children underwent surgery on their primary tumor, while three received stem cell transplants and 10 radiotherapy. Imaging showed that all but one of the patients were clearly responding to treatment. One child’s cancer progressed, two relapsed, and one sadly died — but 10 patients are still alive. Although combining cancer treatments carries a risk of increasing the treatment toxicity, pazopanib was also very well tolerated, with minimal, treatable side-effects.
The scientists calculated a two-year overall survival rate of 85.7%, while 68.2% of patients made it to the end of the second year without a new ‘event’, meaning their cancer remained stable. This is a better result than a previous study on adult patients, suggesting that pazopanib could be more effective and better tolerated in children, or when given earlier in the treatment course.
However, the researchers stress that much more work needs to be done in larger patient groups to validate these exciting early results. Multi-metastatic Ewing sarcoma is rare, so there are few large-scale randomized clinical trials targeting it. But while new treatments are in development, the researchers encourage the scientific community to test the use of pazopanib as an option to help children with severe metastases further.
“While the results are encouraging, larger controlled trials are needed before changing standard practice,” said Raciborska. “Our study could serve as a basis for creating prospective, multicenter clinical trials to confirm these promising results. However, this requires a lot of work and the commitment of resources. Perhaps future EU programs will allow it. We hope that this will be possible.”



 International
International