News release
From:
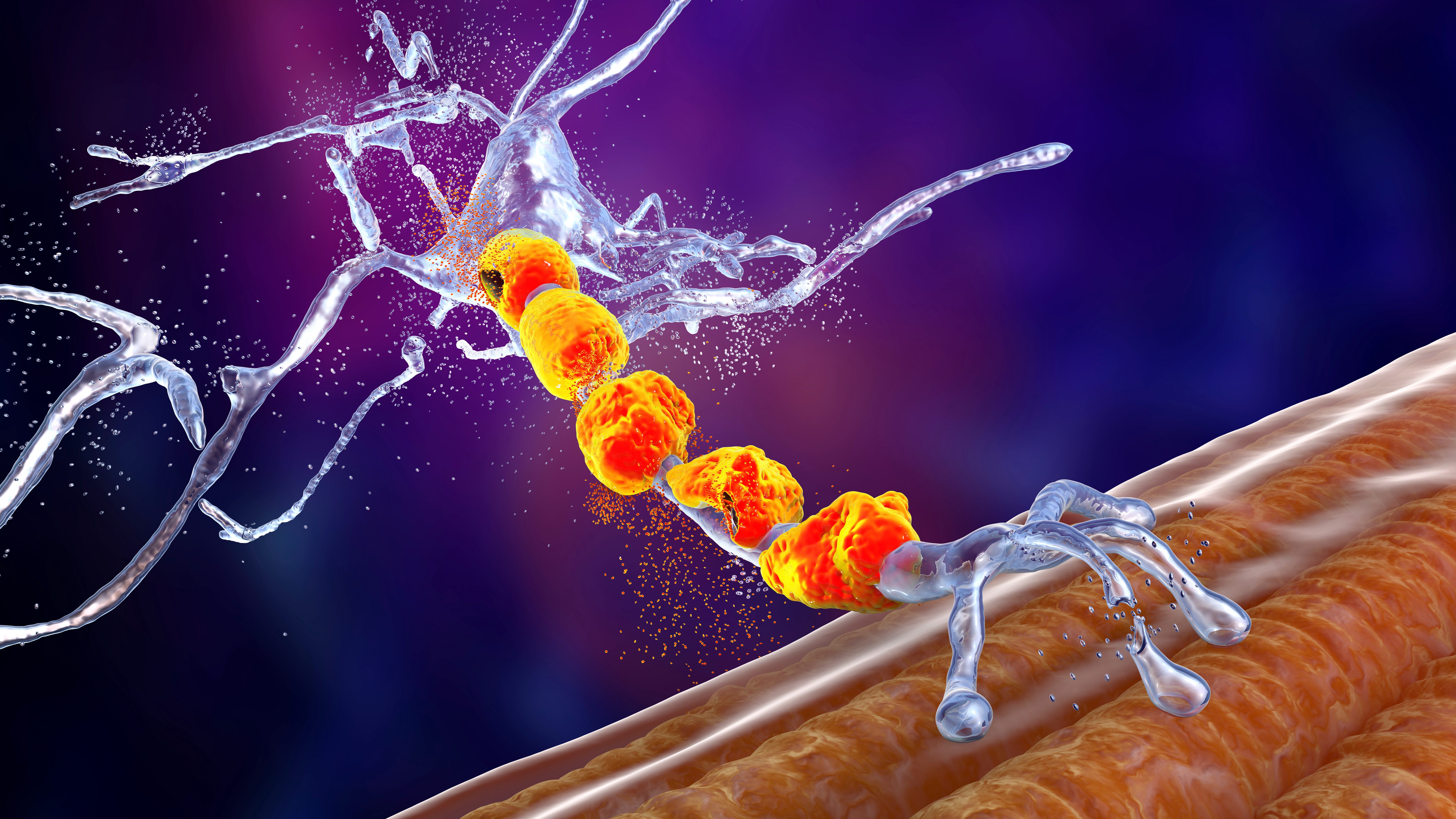
New research at The University of Queensland could help develop viable treatments - and ultimately a cure - for motor neuron disease (MND).
Dr Adam Walker and co-authors Dr Rebecca San Gil, Dr Wei Luan and PhD student Sean Keating from the Queensland Brain Institute have identified biochemical changes in a protein that is affected by MND.
“TDP-43 is a protein found in every cell of the body but is particularly important for the health of motor neurons, the brain cells that control voluntary muscle movement,” Dr Walker said.
“We ran two research projects, looking at how TDP-43 proteins become dysfunctional in motor neurons.
“We found diseased versions of TDP-43 can damage healthy versions of the protein, which may create a cycle of protein dysfunction and degeneration over time.
“We also discovered that biochemical pathways which control neuron death are triggered early, even before MND symptoms begin.
“To change the course of the disease we need pharmaceutical drugs that can prevent neuron death and this TDP-43 protein dysfunction.”
The research used genetic engineering technology called CRISPR, which is a gene editing tool.
“It allowed us to see TDP-43 in live cells for the first time,” Dr Walker said.
Co-author Sean Keating said the research also found neural pathways change as MND progresses, indicating the potential need for different treatments at different phases of the disease.
“We are now treating genetically modified mice with MND with different pharmaceutical drugs that specifically target the underlying causes of the disease, and correct the disease mechanism,” Mr Keating said.
“Our aim is to stop the TDP-43 degenerative cycle and halt the progression of the disease.
“This research improves our understanding of MND, and we hope it will play an important role in the fight against the disease.”
The research was supported by grants and investment from FightMND, the Maclean Family, the Thornton Foundation, MND Research Australia and the Brazil Family Program for Neurology.
The research was published in Molecular Psychiatry and Cellular and Molecular Life Sciences.



 Australia; QLD
Australia; QLD