Media release
From:
The Lancet: Three in five liver cancer cases due to preventable risk factors; obesity-linked cases on the rise, new analysis suggest
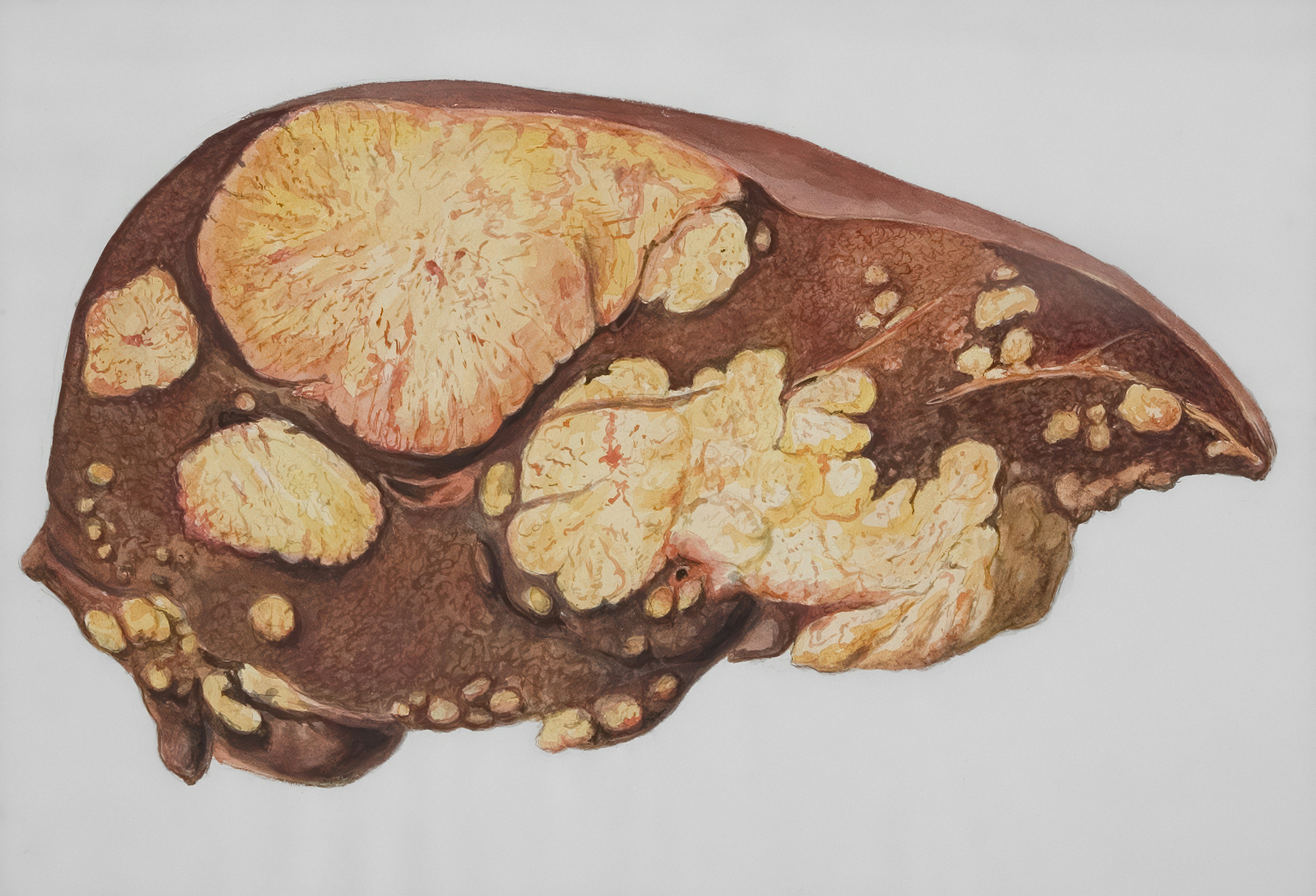
- Over 60% of liver cancers globally are preventable through reduction of risk factors including viral hepatitis, alcohol and metabolic dysfunction-associated steatotic liver disease (MASLD) - a long-term liver condition caused by excess fat in the liver.
- The Lancet Commission on liver cancer predicts the share of liver cancer cases caused by a severe form of MASLD called metabolic dysfunction-associated steatohepatitis (MASH) will increase by 35% (8% to 11%) by 2050.
- The authors call for increased public, medical and political awareness of the rising risk of MASLD – especially in USA, Europe and Asia - with a focus on high-risk groups, including individuals with diabetes and obesity.
- With the number of new liver cancer cases predicted to double over the next 25 years without urgent action, the Commission sets the target of an annual reduction of 2% to 5% in the number of new cases - preventing up to 17 million liver cancer cases and up to 15 million deaths, if achieved.
The majority of liver cancer cases could be prevented by reducing levels of viral hepatitis, alcohol consumption and MASLD (metabolic dysfunction-associated steatotic liver disease – previously called non-alcoholic fatty liver disease), suggests an analysis as part of The Lancet Commission on liver cancer. The Commission highlights several ways to reduce these risks factors, including increasing the coverage of the hepatitis B vaccine and public health policies targeting obesity and alcohol consumption.
Previous analyses have predicted that the number of new liver cancer cases will nearly double from 870,000 in 2022 to 1.52 million in 2050, primarily due to population growth and ageing populations, with the largest increases expected in Africa. The number of deaths from liver cancer are predicted to grow from 760,000 in 2022 to 1.37 million in 2050. [1]
Liver cancer is already a major cause of death and disability. Globally, it’s the sixth most common cancer and the third leading cause of death from cancer. More than 40% of the global liver cancer cases occur in China, mostly due to relatively high rates of hepatitis B infections in the country.
Chair of the Commission, Prof Jian Zhou, Fudan University (China) says: “Liver cancer is a growing health issue around the world. It is one of the most challenging cancers to treat, with five-year survival rates ranging from approximately 5% to 30%. We risk seeing close to a doubling of cases and deaths from liver cancer over the next quarter of a century without urgent action to reverse this trend.”
First author, Prof Stephen Chan, Chinese University of Hong Kong (Hong Kong, China) adds, “As three in five cases of liver cancer are linked to preventable risk factors, mostly viral hepatitis, alcohol and obesity, there is a huge opportunity for countries to target these risk factors, prevent cases of liver cancer and save lives.”
Changes in the causes of liver cancer
In a novel analysis, the Commission estimates that at least 60% of liver cancers are preventable via control of modifiable risk factors, including hepatitis B virus (HBV), hepatitis C virus HCV, MASLD, and alcohol.
MASH, a severe form of MASLD, is the fastest growing cause of liver cancer globally, followed by alcohol. The Commission projects that the proportion of liver cancer cases associated with MASH are projected to increase from 8% in 2022 to 11% in 2050, and liver cancer cases associated with alcohol are projected to increase from 19% in 2022 to 21% in 2050
In contrast, the proportion of liver cancer cases linked to HBV is expected to decrease from 39% in 2022 to 37% in 2050, while HCV-related cases are projected to drop from 29% to 26% over the same period.
A rising risk factor: MASLD
Approximately a third of the global population are estimated to have MASLD. However, only 20 to 30% of patients with MASLD develop the more severe form of the condition with liver inflammation and damage - called metabolic dysfunction-associated steatohepatitis (MASH).
The rate of MASLD-linked liver cancer is expected to rise over the next decade, particularly in the USA, Europe, and Asia, due to increasing rates of obesity. In the USA, MASLD prevalence continues to climb in parallel with the obesity epidemic; by 2040, over 55% of US adults could have MASLD. [For a case study from the USA: ‘MASLD and ALD as the new face of hepatocellular carcinoma’ – see panel 5, page 17 of the report.]
Commission author, Prof Hashem B El-Serag, Baylor College of Medicine (USA) says, “Liver cancer was once thought to occur mainly in patients with viral hepatitis or alcohol-related liver disease. However, today rising rates of obesity are an increasing risk factor for liver cancer, primarily due to the increase in cases of excess fat around the liver.
“One approach to identify patients at high risk of liver cancer would be to introduce screening for liver damage into routine healthcare practice for patients at high risk of MASLD, such as individuals living with obesity, diabetes, and cardiovascular disease. Healthcare professionals should also integrate lifestyle counselling into routine care to support patients to transition to a healthy diet and regular physical activity. Furthermore, policy makers must promote healthy food environments via policies such as sugar taxes and clear labelling on products with high fat, salt, and/or sugar.”
Global targets and recommendations
The Commission estimates that if countries can reduce the incidence of liver cancer cases by 2 to 5% each year by 2050, it could prevent nine to 17 million new cases of liver cancer and save eight to 15 million lives.
As more patients live with liver cancer than ever before, in addition to prevention efforts, there is an urgent need for increased research and attention for these patients to improve their quality of life.
The Commission suggests several strategies for reducing the global burden of liver cancer, including:
- Governments should intensify efforts to increase HBV vaccination—such as vaccine mandates in high-prevalence countries—and implement universal HBV screening for adults 18+, alongside targeted HCV screening in high-risk areas based on cost-effectiveness.
- Policy makers should enact minimum alcohol unit pricing, warning labels, and advertisement restrictions for alcoholic beverages.
- National health authorities and cancer control programmes should prioritise investments in public awareness campaigns and deployment of early detection resources.
- Professional organisations and the pharmaceutical industry should work together to reduce differences between Eastern and Western regions of the world in the clinical management of liver cancer.
- Hospitals and professional organisations should provide palliative care training, with the aim of integrating palliative care in the early phases for patients in need.
- [For a full list of the Commission’s ten recommendations for action see table 1, page 4]
Commission author, Prof Valérie Paradis, Beaujon Hospital (France) says, “There is an urgent need to raise awareness within society about the severity of the growing health issue of rising liver cancer cases. Compared with other cancers, liver cancer is very hard to treat but has more distinct risk factors, which help define specific prevention strategies. With joint and continuous efforts, we believe many liver cancer cases can be prevented and both the survival and quality of patients with liver cancer will be considerably improved.”




 International
International