News release
From:
Elevated Lipoprotein(a) is the latest variant of ‘bad cholesterol’ found to increase the risk of recurrent coronary heart disease
Future therapeutics to reduce elevated Lp(a) might help prevent recurrent disease
Increased levels of Lipoprotein(a), a variant of ‘bad cholesterol’, in the bloodstream are a risk factor for recurrent coronary heart disease (CHD) in people aged 60 or over, according to the results of a new study which tracked the issue over the course of 16 years.
The results, published today in Current Medical Research & Opinion, suggest that current cholesterol-lowering medications may not be effective at reducing the risk of recurrent CHD – such as a heart attack – due to elevated Lp(a).
“This finding adds to growing evidence of a relationship between increased Lp(a) and the risk of recurrent CHD,” says lead author Associate Professor Leon Simons, from the School of Clinical Medicine, at the University of New South Wales Sydney. “It is well-established that people who have already experienced CHD are at very high risk of another event. Our new results indicate that new therapeutics in development that aim to reduce elevated Lp(a) might help prevent recurrent disease. However, the potential clinical benefit of therapy to reduce elevated Lp(a) is yet to be confirmed.”
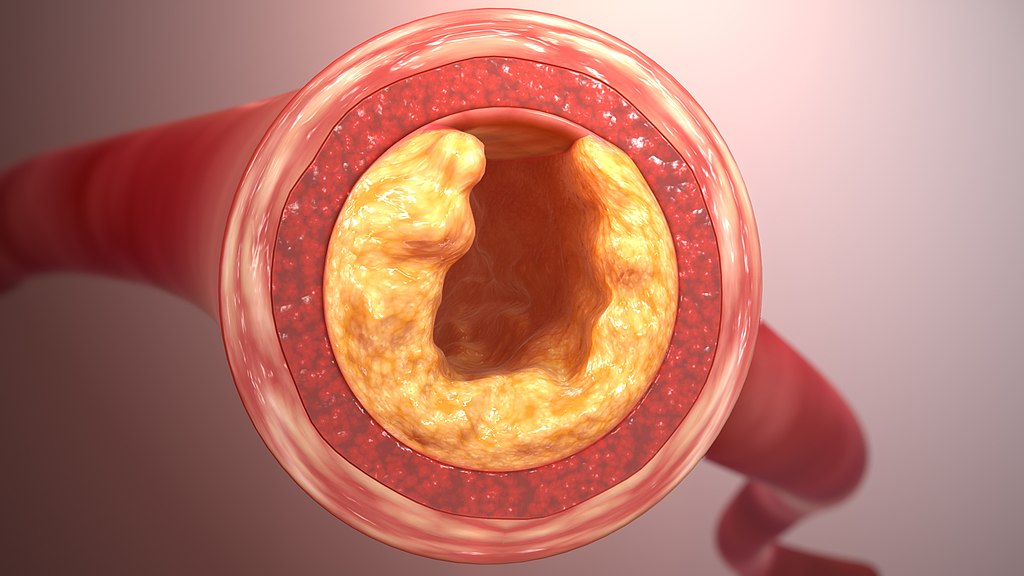
CHD is the most common type of heart disease. It occurs when the arteries that supply the heart with oxygen-rich blood become narrowed by a build-up of fatty material within their walls. It is the most common cause of heart attack and was the single biggest killer of both and men and women worldwide in 2019.
High levels of cholesterol in the blood can increase the risk of CHD. Cholesterol travels through the blood on lipoproteins, which are made of protein and fat. Lipoproteins include low-density lipoprotein (LDL), high-density lipoprotein (HDL) and Lp(a). LDL cholesterol is often called ‘bad cholesterol’ because it collects in blood vessel walls, increasing the chances of cardiovascular disease. Lifestyle changes and/or medications, like statins, may help to get a person’s cholesterol numbers into the healthy range.
While previous research has indicated that high levels of Lp(a) are also an important risk factor in the development of CHD, most of these studies have looked at Lp(a) levels and the risk of a first CHD event. The current study looked at whether elevated Lp(a) is predictive of a second or recurrent CHD event. It involved 607 Australians aged 60 years and over, all with prevalent CHD, who were followed for 16 years as part of the Dubbo study. There were 399 incident CHD cases.
The researchers found that:
- The median Lp(a) in people who had a recurrent CHD event was 130 mg/L, compared to 105 mg/L in those who did not.
- 26% of people who had a recurrent CHD event – and 19% of those who did not – had Lp(a) levels of >300 mg/L.
- 18% of people who had a recurrent CHD event – and 8% of those who did not – had Lp(a) levels of >500 mg/L.
In senior citizens with prior CHD, elevated Lp(a) in the top 20% of the population distribution (>355 mg/L) predicted a 53% excess risk of a recurrent CHD event, compared with those in the lowest 20% of the population distribution (<50 mg/L) over 16 years of follow-up. This prediction was independent of other risk factors.
"We conclude that elevated Lp(a) is an important predictor of recurrent CHD in older people. Upper reference Lp(a) levels of 500 mg/L or 300 mg/L both appear to be appropriate for identifying those at higher risk who may benefit from more intensive risk reduction interventions,” says Associate Professor Simons. “While current medications, such as statins, are often prescribed to lower ‘bad cholesterol’ in patients at higher risk of cardiovascular disease, these do not have any major or proven impact on elevated Lp(a). But there is hope for the future – as some novel therapeutics that are designed to lower the levels of Lp(a) are currently in the advanced stages of clinical development.”
A key limitation of this longitudinal study is that the baseline data were collected in 1988-89. However, while there may have been other influences affecting CHD risk over the years of follow-up, especially with the use of statin therapy, it can be reasonably assumed that people with elevated Lp(a) at the start of the study will maintain that status during the whole period.



 Australia; NSW
Australia; NSW