News release
From:
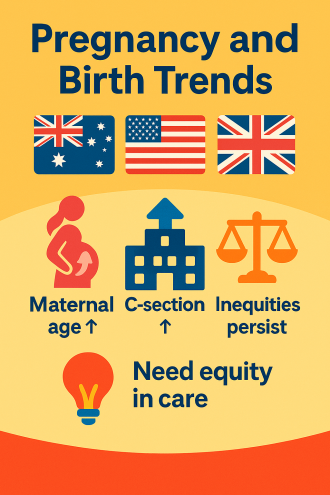
Women across Australia, the United States (USA) and the United Kingdom (UK) are having babies later in life, and a new international study warns that this shift brings rising health risks and widening inequalities in maternal care.
The review, led by researchers at Flinders University and published in the Journal of Clinical Medicine, explores how pregnancy and birth have changed in Australia, the USA and UK over the past twenty years.
“One of the most noticeable shifts is that women are having babies later in life,” says lead author, Dr Anya Arthurs, from Flinders University.
“The average age of first-time mothers has steadily increased, with many now starting their families aged 35 years or over, reflecting broader societal changes including career priorities, financial pressures and improved access to contraception.”
Dr Arthurs explains that while older mothers are more likely to engage with prenatal care, they also face higher risks of complications.
“We’re seeing increased rates of gestational diabetes, high blood pressure and caesarean sections among older mothers, which raises important questions about how maternity care systems are adapting,” she says.
The study also found that fertility rates are falling in all three countries, with birth rates now below the level needed to maintain population size without immigration. This decline is linked to economic factors, changing family structures and personal choices.
Despite the overall drop in births, the number of babies born to Indigenous and minority women is increasing, however these groups continue to face significant health disparities.
“Maternal mortality remains a serious concern, especially in the USA, where Black, Indigenous and Hispanic women are far more likely to die during pregnancy or childbirth due to limited access to quality healthcare and systemic inequalities,” says Dr Arthurs.
Whilst maternal deaths are comparatively lower in Australia and the UK, there are troubling gaps in care for Indigenous women in Australia and migrant women in the UK, leading to worse outcomes.
The COVID-19 pandemic added further strain to maternity care systems and, in the UK, it became a leading cause of death among pregnant women caused by disruptions to prenatal services and hospital care, especially for women already facing disadvantage.
The review also found a rise in caesarean sections, particularly among older mothers and those giving birth in private hospitals, which may reflect personal choice or systemic factors rather than providing better clinical outcomes.
Gestational diabetes and high blood pressure during pregnancy are also on the rise and more common among older mothers and certain ethnic groups, contributing to potentially concerning health issues for both mother and baby both in the short and long-term.
Dr Arthurs says that there are some encouraging trends. “Smoking during pregnancy is declining across all three countries, and breastfeeding rates are improving, especially in Australia and the UK,” she says.
“But younger mothers are still more likely to smoke, and the USA continues to lag in breastfeeding rates, partly due to the absence of a national paid maternity leave policy.”
Senior researcher and author on the study, Professor Claire Roberts, says that the findings underscore an urgent need for equity-focused, culturally safe, and system-level interventions, as well as improved data collection and international collaboration to reduce preventable harms.
“We’re calling for governments and health systems to take action by focusing on maternity care that is equitable, culturally safe and responsive to changing needs,” says Professor Roberts from Flinders Health and Medical Research Institute (FHMRI).
The authors of the review have the following policy recommendations:
- Governments should set national targets to reduce maternal mortality and stillbirth rates, supported by dedicated funding for underserved populations.
- Australia and the USA should adopt the UK’s midwifery-led continuity of care model to improve maternal satisfaction and reduce interventions.
- The UK and Australia should implement the USA’s detailed public reporting of maternal outcomes by race, ethnicity, and social determinants.
- Culturally safe perinatal programs like Australia’s Birthing on Country should be expanded and adapted for Indigenous and minority communities in the USA and UK.
- All three countries should introduce anti-racism and structural competency training for maternity care providers to address bias in clinical decision-making.
- Health systems should revise funding models that incentivise caesarean sections and instead promote value-based, woman-centred care.
- The USA should implement universal paid parental leave to support maternal and infant health, following models in Australia and the UK.
- Postpartum care should be improved, especially for women with gestational diabetes or hypertensive disorders, to manage long-term health risks.
- Governments should address social determinants of health, including housing, income, and food security, to improve pregnancy outcomes.
- An international maternal health equity taskforce should be established to coordinate global efforts and reduce disparities in maternal care.
The paper, ‘Pregnancy and Birth Trends Across Australia, the United States of America and the United Kingdom’ by Anya L. Arthurs, Jade K. Harrison, Jessica M. Williamson and Claire T. Roberts was published in Journal of Clinical Medicine. DOI: https://doi.org/10.3390/jcm14165841
Acknowledgements: A.L.A. is supported by a Future Making Fellowship from the University of Adelaide and funding from the Channel 7 Children’s Research Foundation. C.T.R. is supported by an NHMRC Investigator Grant (GNT1174971) and a Matthew Flinders Fellowship from Flinders University.
Multimedia




 Australia; International; SA
Australia; International; SA



