Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Dr Georgia Rigas is a VMO-Obesity Doctor & Senior Bariatric Medical Practitioner at St George Private Hospital, Kogarah and consulting also at Cronulla. She is the founder & past chair of the RACGP Obesity Management Network
Interpret this research letter with caution.
Those already on anti-obesity treatment should not stop their medication, especially if they have no symptoms or side-effects, however, should speak to their doctor if they have any concerns. Patients considering starting anti-obesity treatment should have an in-depth assessment and subsequent discussion with a doctor experienced in managing people living with overweight/obesity so that any recommendations are tailored to the patient's individual health profile.
Nothing we do/take or decide to not do/take is without risk. The key is patients need to be informed of what the medical evidence tells us, have it put it into context, with a goal to assist them in making an informed decision. Furthermore, empowering patients with a list of 'what to look out for' and what to do about it if they develop symptoms during and out of office hours.
As the incidence of these complications is low, we can still prescribe as is clinically indicated, however as with all prescribed and over the counter preparations, we still need to remain vigilant.
Peter Clifton is an Adjunct Research Professor of Nutrition at the University of South Australia
The paper is a timely reminder that there are potentially rare side effects with this class of drugs. Despite the very wide use of these drugs, the number of patients examined and the number of events are low and the confidence intervals very wide. Weekly semaglutide may cause fewer problems than daily liraglutide, but the duration of use is shorter. This research should prompt further examination of adverse event reporting in Australia.
Dr Ian Musgrave is a Senior Lecturer in the Faculty of Medicine, School of Medicine Sciences, within the Discipline of Pharmacology at the University of Adelaide.
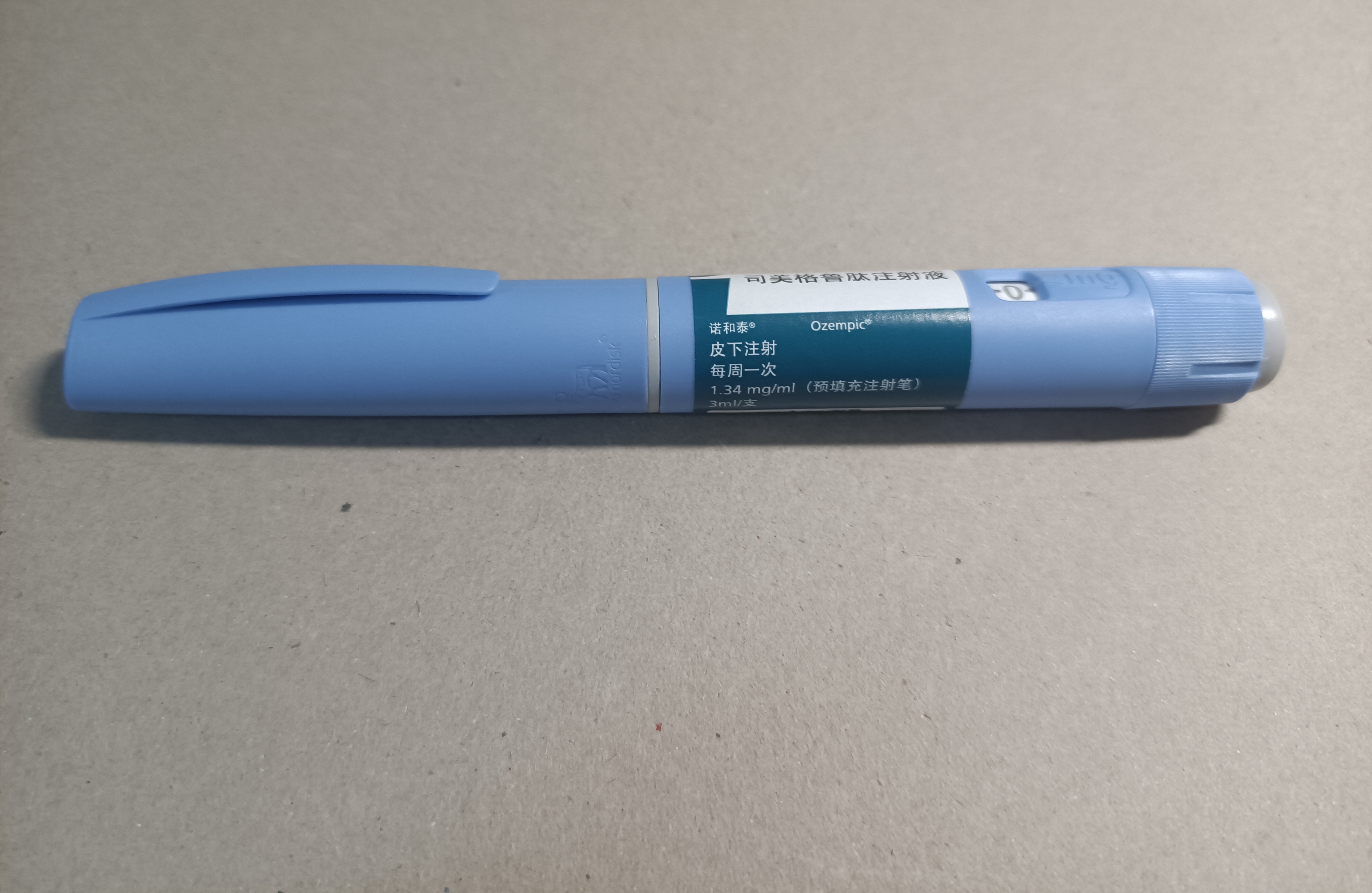
Glucagon Like Peptide-1 agonists (GLP-1 agonists) such as Ozempic mimic hormones that link the absorption of nutrients from the gastrointestinal tract with pancreatic hormone secretion and help regulate insulin release after eating. They are a useful add-on therapy for type 2 diabetes. As well as lowering blood glucose, they also have other favourable effects such as reducing blood pressure and providing protection for the heart and kidneys.
As well, they have multiple effects such as increased satiety, decreased appetite and decreased gastric motility that results in weight loss. As a result, off label prescription of these drugs for weight loss has increased to the point that in the UK there is a shortage of GLP-1 agonists for type-2 diabetes that is expected to last until 2024.
While GLP-1 agonists are generally well tolerated, there is a low incidence of serious side effects. For example, pancreatitis (inflammation of the pancreas) is a known side effect of these agents in patients with for type-2 diabetes. However, the incidence of serious side effects in people using GLP-1 agonists for weight loss is unclear.
This paper attempts to clarify gastrointestinal side effects in people taking GLP-1 agonists for weight loss by comparing them to people taking another pharmaceutical intervention. This was a well-conducted study comparing two long acting GLP-1 agonists (Ozempic and Victoza) to naltrexone-bupropion taken for weight loss. However, there were far more GLP-1 agonists patients than naltrexone-bupropion patients, this may affect the findings. The study took into account factors such age, sex, alcohol use, smoking, hyperlipidemia, abdominal surgery, and geographic location but did not compare effects of body mass index.
Compared to people on naltrexone-bupropion, people on GLP-1 agonists were more likely to have pancreatitis, delayed gastric emptying and bowel obstruction. This is consistent with what is known from studies on patients with type-2 diabetes. These findings will assist with prescribing these agents for weight loss (eg advising people with a history of pancreatitis or delayed gastric emptying to avoid these agents). Any choice of pharmacological agent to assist with weight loss must be carefully considered, balancing benefits and side effects. For example, naltrexone-bupropion has a lower incidence of serious gastrointestinal side effects compared to GLP-1 agonists, it also has side effects that must be carefully considered such as seizures, high blood pressure and suicidal thoughts or actions.
Associate Professor Priya Sumithran is from the Central Clinical School at Monash University and the Department of Endocrinology and Diabetes, Alfred Health
This letter reports data from a health claims database for people with a recent diagnosis of obesity who were prescribed semaglutide, liraglutide or bupropion-naltrexone. The analysis found that a diagnosis of pancreatitis, bowel obstruction or gastroparesis (or being prescribed a medication to speed up emptying of the stomach) were more common in people prescribed liraglutide or semaglutide compared with bupropion-naltrexone.
The authors conclude that these adverse events must be considered by patients who are considering using the medications for weight loss. In this study, it isn’t possible to be sure whether the medications were prescribed for weight loss. Regardless of whether medications are being prescribed for obesity, diabetes or other conditions, their risks and benefits should always be considered in relation to the goals and needs of the individual patient.
It is worth noting that the vast majority of patients in the analysis were prescribed liraglutide. Although the analyses combined patients prescribed liraglutide and semaglutide, the numbers of patients with the gastrointestinal diagnoses were very small for semaglutide (0-4).
Professor Gary Wittert is from the Adelaide Medical School at the University of Adelaide
The gastrointestinal adverse effects of GLP-1 receptor agonists are well documented in the clinical trials done to date. This analysis from a large health claims database, confirms the increased risk, but it is rare. For example, pancreatitis occurred in 0.46% of users of semaglutide.
The use of Bupropion-Naltrexone as a comparator is perplexing because compared to semaglutide it has a limited effect on weight. Furthermore, bupropion-naltrexone has its own set of adverse effects, and compared to GLP-1 receptor agonists, a far more limited benefit for glycaemia and there are no data showing cardiovascular or renal benefits.



 Australia; International; NSW; VIC; SA
Australia; International; NSW; VIC; SA