News release
From:
Bypassing the base: mRNA vaccines for HIV produce potent immune responses and show promise in humans
Science Translational Medicine
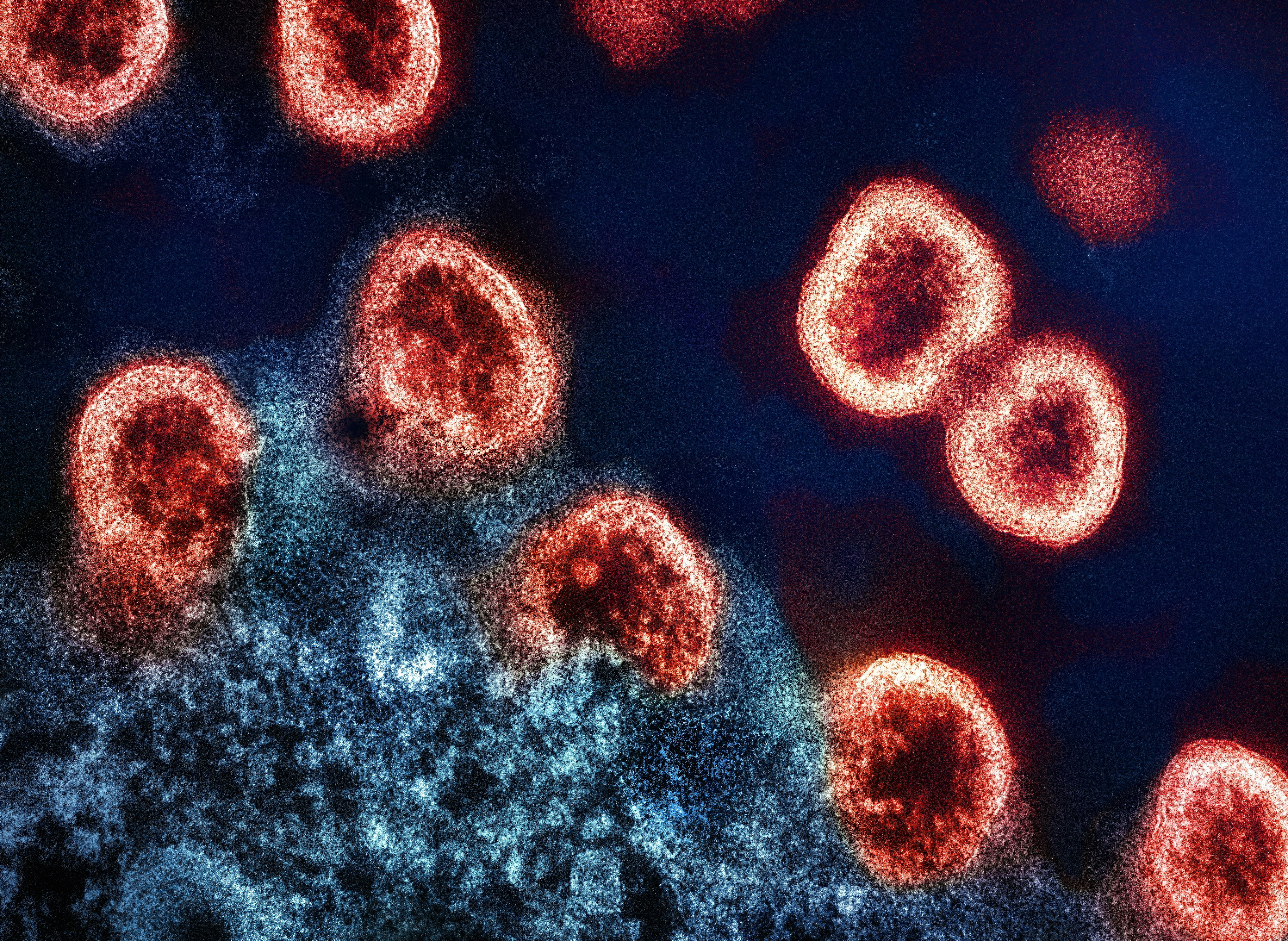
In a pair of new studies, researchers have applied mRNA technology to engineer new vaccines for HIV, which produced potent immune responses in animals and human volunteers. By using mRNA to bypass a common design obstacle with HIV vaccines, the experiments underscore the utility of this platform in the quest for more effective and affordable vaccines for HIV and other diseases. Current vaccine candidates for HIV are largely based on the HIV envelope (Env) trimer and require it to be soluble (or not bound to cells). However, this exposes the base of Env to antibodies, even though the base is normally embedded in the HIV virion and is hidden from immune cells. As a result, antibodies that target the Env base don’t protect against infection. Parham Ramezani-Rad and colleagues theorized they could solve this problem with mRNA technology, which also offers superior production speed and lower costs. They tested two vaccines: one that delivers a soluble form of a stabilized Env trimer, and a second that instead delivers a membrane-bound form of Env.
This second form can be produced directly in the vaccine recipient’s cells and is displayed on the membrane, thus shifting the immune system’s attention away from the Env base and towards the proper target. When tested in rabbits and macaques, the membrane-bound vaccine elicited stronger neutralizing antibodies and reduced off-target responses toward the Env base. In the second study, Katherine Parks and colleagues built on these findings and evaluated the safety and preliminary effects of three mRNA vaccines in a phase 1 clinical trial. The researchers enrolled 108 healthy volunteers and administered three immunizations of mRNA encoding either a soluble Env trimer or a membrane-anchored Env trimer. Overall, the volunteers tolerated the vaccines well, and there were no major adverse effects besides a higher-than-average incidence of hives (6.5%). The membrane-anchored trimer vaccine generated neutralizing antibodies in 80% of the vaccinees, while the soluble trimer vaccine generated the same antibody response in only 4% of recipients. “With demonstration of more favorable safety, mRNA-encoded membrane-anchored HIV envelope trimers represent a promising platform for HIV vaccine clinical development,” Parks et al. conclude.
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Associate Professor Seth Cheetham is Deputy Director of the BASE mRNA Facility at The University of Queensland
This study marks significant progress in the global effort to develop a safe and effective HIV vaccine that prevents infection. While drugs for HIV treatment and prevention have transformed the lives of people living with HIV, an effective vaccine is still urgently needed.
mRNA, the technology behind many of the COVID-19 vaccines, dramatically speeds up the pace of vaccine development. This enables researchers to have more ‘shots on goal’, opening the door to tackling even the most complex viruses like HIV.
Researchers from the Fred Hutchinson Cancer Center tested a new type of HIV vaccine that uses a new approach. By displaying a part of the virus on the surface of cells, the immune system can recognise it. This teaches the body to create antibodies that can effectively block infection.
In the early-stage clinical trial, the results were encouraging: 80% of people who received this version of the vaccine produced antibodies that could block the virus in lab tests. That’s a big improvement compared to most earlier vaccine candidates, which were less targeted and rarely triggered these strong immune responses.
The vaccine also generated strong memory responses, meaning the body would be better prepared to fight off HIV even long after vaccination. While most adverse reactions were mild and treatable, several people experienced a skin reaction (urticaria). If these side effects can be reduced in next-generation versions and the results hold up in larger real-world studies in the community, mRNA vaccines could be a transformative tool in the fight against HIV.



 International
International