News release
From:
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Professor Paul Griffin is the Director of Infectious Diseases at Mater Health Services and the Head of the Mater Clinical Unit for the University of Queensland School of Medicine
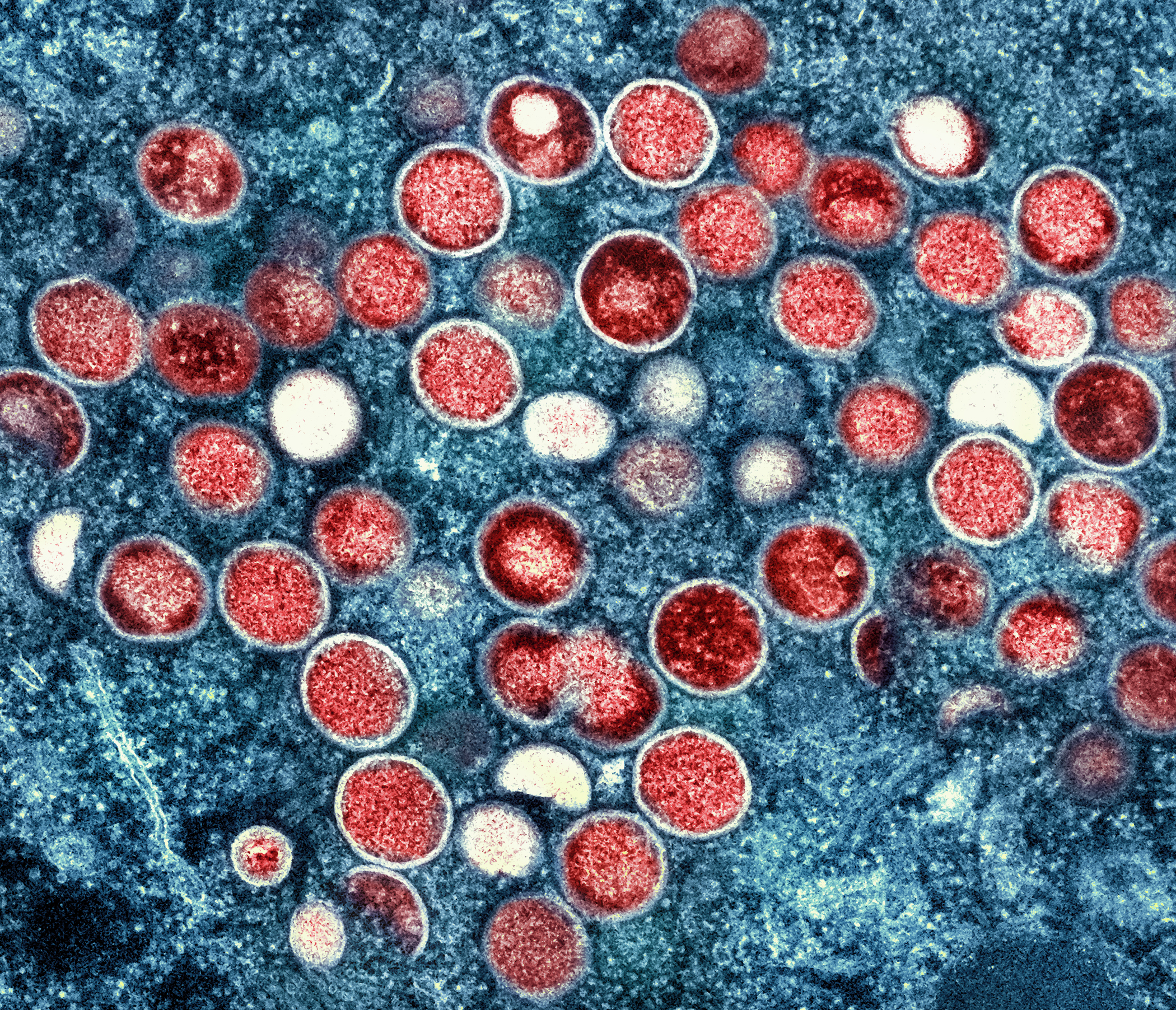
Q: Now that the WHO has declared the spread of monkeypox a public health emergency and Australia’s CMO has declared it a “communicable disease incident of national significance”, is it time to worry?
"I don’t think we should encourage anyone to be worried necessarily. What we need here is a perception of risk that’s sufficient that appropriate awareness is widespread. There are a number of very reassuring considerations when it comes to Monkeypox.
Whilst the situation now is truly extraordinary with over 20 000 cases globally, its actually an infection that’s relatively hard to transmit. The fact that people with this infection are often visibly unwell with a rash, should also make it a little easier to identify them.
We also already have safe and effective vaccines as well as therapies, so our tools to combat this infection are far more advanced than they were for COVID-19 for example at the beginning of the pandemic.
I certainly welcome both the Australian decision to declare this a communicable disease incident of national significance and the WHO’s declaration that this incident is a global health emergency as this should facilitate the required awareness as well as a more coordinated response to improve on these tools and make sure our ability to manage this incident is further improved but these announcements should not be cause for worry or panic."
Q: Do these declarations imply that we are on the verge of another pandemic?
These declarations do indicate the significance of the event and should hopefully be the catalyst to facilitate an efficient and more effective response to hopefully bring the situation under better control but in no way indicate that this is going to lead to the next global pandemic.
Fortunately this virus is harder to transmit than COVID-19, for example, requiring direct contact with infected blood or body fluid. It also most often leads to an illness that’s visible as the rash is quite prominent, so infected individuals are relatively less likely to go about their normal lives whilst infectious, particularly if they understand the significance of this infection and receive the right advice to isolate.
Hopefully the recent declarations should highlight the significance of this event and lead to enhanced communication and awareness both of the public and clinicians so our ability to find cases early and then isolate them is improved.
It should also make sure we have coordinated policies and procedures to ensure our control is optimised. We also need to make sure we get the vaccines that are highly effective but still a little limited in supply to where they will have the greatest benefit.
Hopefully, this will also lead to research so we can better understand why the virus has quickly become so widespread and this will potentially further increase our ability to contain it moving forward."
Q: What should people be doing to avoid becoming infected? Do similar protocols used for COVID-19 (mask wearing, social distancing, hand sanitising etc) work for the virus responsible for monkeypox?
"Given this virus is so different to COVID-19, the measures required to manage it are quite different. The number one priority is finding cases as early as possible. This should hopefully be improved if the general public as well as clinicians understand who is currently at greatest risk and what symptoms to look out for.
If anyone is at all suspicious they may be infected, the first step should be to contact the appropriate authorities to alert them and facilitate testing. This could your local GP, local public health unit or hospital potentially depending on where you are.Cases should then isolate as directed by their relevant public health units.
Understanding who is currently at greatest risk is a good way of being able to reduce that risk. The majority of cases so far have been in men who have sex with men and there have often been additional risk factors such as large parties where at risk activities are undertaken or sex on premises venues for example where people may have close physical contact with a relatively large number of other people.
Those at highest risk could be considered for vaccination but most importantly should just be cautious about contact with an infected individual. The risk of this happening of course is less if we find cases early and isolate them.
High risk close contacts can also be considered for vaccination as a way of reducing their risk of becoming infected. Basic infection control strategies including using personal protective equipment if you are caring for someone who is infected and hand hygiene can also further reduce the risk."



 Australia; QLD
Australia; QLD