Media release
From:
Screening for cervical abnormalities in women offered HPV vaccination: comparing HPV testing with cytology
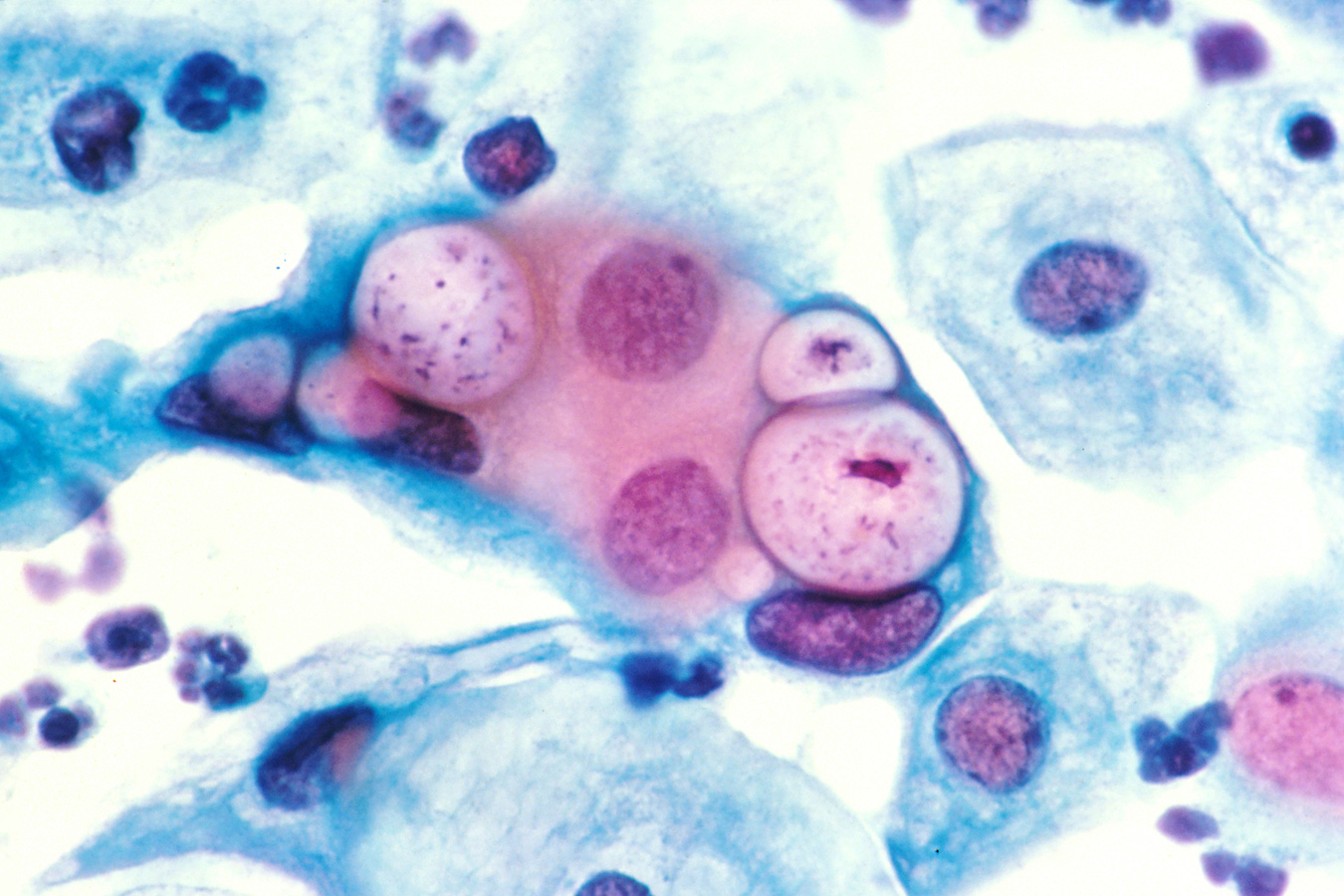
Human papillomavirus (HPV) testing detects a higher number of precancerous cervical lesions than cytology-based Pap smears in a female population including a proportion offered HPV vaccination, according to a new study published in PLOS Medicine by Karen Canfell of Cancer Council New South Wales, Australia, researchers at the Victorian Cytology Service, Melbourne, Australia, and colleagues.
Many countries are currently considering switching from classic Pap tests to primary HPV tests for cervical cancer screening, based on the strong evidence linking cervical abnormalities and infection with certain HPV types, and data suggesting that HPV tests detect more high-grade precancerous lesions. However, no study has yet compared the different methods in a population in which younger women had been offered prior HPV vaccination.
In the new Compass pilot study, researchers randomized cervical samples from 4,995 women aged 25–64 in Australia, in a 1:2:2 ratio, to be analyzed by either cytology (with HPV testing of low-grade abnormalities), HPV testing with partial genotyping of the virus for the highest risk types HPV16 and 18, and cytology (for participants with other high-risk HPV genotypes), or HPV testing with partial genotyping and dual-stained cytology. In the first screening round of the trial, the authors assessed the rates of women being referred for further testing and of detection of CIN2+ (high-grade cervical intraepithelial neoplasia) precancerous lesions.
For the cytology group, the overall referral and detected CIN2+ rates were 27/995 (2.7% [95%CI 1.8–3.9]) and 1/995 (0.1% [95%CI 0.0–0.6]), respectively; for the HPV testing and cytology group these were 75/1992 (3.8% [95%CI 3.0–4.7]) and 20/1992 (1.0% [95%CI 0.6–1.5]); and for the HPV and dual-stained cytology group these were 79/2008 (3.9% [95%CI 3.1–4.9]) and 24/2008 (1.2% [95%CI 0.8–1.6]). The researchers found that, in the first round of screening, detection of CIN2+ was significantly increased with HPV testing as compared with cytology, while referral was non-significantly increased. Adverse events were rare, and the one case of early-stage cervical cancer (in the HPV testing plus cytology group) was detected as appropriate by screening.
“These findings provide initial confirmation of an improved performance of primary HPV screening compared to cytology screening in settings with HPV-vaccinated populations,” said Dr. Canfell. These findings support the planned imminent introduction of cervical screening by HPV testing in Australia which will occur at the end of 2017.
Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Prof Rachel Skinner is an HPV and vaccination researcher, and Professor of Paediatrics & Child Health at the University of Sydney
This research is the first study in Australia to evaluate how well HPV DNA testing detects cervical high-grade precancerous disease compared with standard Pap tests (Liquid-based cytology). It is the first study in the world to undertake this comparison in a population of young women, most of whom have been vaccinated against HPV 16 and HPV 18.
The study found that HPV testing was superior to cytology in the detection of high-grade precancerous disease in women who were in the vaccinated age group as well as in older unvaccinated age group. The researchers found that HPV testing detected about 10 times more disease than regular cytology.
This research is very important for Australia cervical screening programs as it provides empirical evidence on the superiority of HPV screening in an Australian context right at the time when our cervical screening program will be changing from cytology to HPV testing. This evidence will reassure clinicians who are offering screening to women and will reassure women who are concerned that about cervical cancer risk.
This research tells that Pap tests are much more likely to miss precancerous cervical disease than HPV testing.
In Australia, screening intervals will be increasing from 2 yearly to 5 yearly. This research should reassure clinicians and women that HPV testing will increase the chance of detection of a precancerous cervical lesion by around 10 fold, and hence should reassure women that, if they are screen negative, repeat testing is not necessary until 5 years. It was also reassuring that in the younger age group, women who had been offered vaccination, the detection rates were also 10 fold higher compared with standard cytology.
Women who have been offered vaccination still need to participate in the cervical screening program as the vaccine does not protect against all cancer causing types of HPV.
Professor Karen Canfell is a cancer epidemiologist and Professor of Public Health at The University of Sydney
This is a world-first piece of research: for the first time ever, a trial is comparing HPV screening with Pap tests in a population where younger women (in their late twenties and early thirties) have been offered the HPV vaccine though a national vaccination program. The study of about 5,000 participants overall found that compared to Pap tests, HPV screening provides significantly increased detection of high-grade cervical abnormalities in this population.
The findings published in PLOS Medicine today come as Australia prepares to transition to a renewed National Cervical Screening Program, which will introduce primary HPV screening. The new system will come into place in December this year, so the study is a timely confirmation of just how effective the new program is expected to be – crucially, not just in unvaccinated women, but also in those who were offered the HPV vaccine.
This adds to existing evidence about how much more effective HPV screening is. We now have a superior method for detecting high-grade cervical precancerous abnormalities – this will provide increased protection to women against developing invasive cervical cancer later in life.
The results represent the first real-life demonstration of how the treatment pathways for primary HPV screening in HPV-vaccinated women can work in practice. In the next phase of Compass, which is Australia’s largest clinical trial, we are recruiting more women in specific age groups so we can obtain more detail on the long-term benefits of screening in Australian women. Women aged 25-38 in Victoria or South Australia may be eligible to participate, and can check www.compasstrial.org.au to find a participating practice in their area.
Professor Suzanne Garland is Director of Microbiology & Infectious Diseases at The Royal Women’s Hospital
Australia has been very much ahead with respect to the national HPV vaccine program, having instituted a government funded school-based program which is being endorsed by general public and clinicians.
This is exemplified by the high coverage rate, and due to that a big reduction in vaccine-related HPV infections and consequent diseases such as genital warts, high grade lesions; the precancerous lesions to cervical cancer which, if adequately treated, prevent development of cancer.
It is for this reason that the government is moving to a more sensitive technology in its strategy for prevention of cervical cancer this year. This new technology utilises molecular biology (HPV DNA) for screening as compared to the old Pap smear (cervical cytology). This study in PLOS Medicine underpins the decision by the government to move from cytology to HPV DNA as of December 1 this year.
The decision by the government was made from results of studies internationally, but the results from this recent randomised controlled trial in Australia, conducted after vaccination which has been implemented now for 10 years, give us confidence that the decision being made to move to HPV DNA (commencing from 25 years of age) is a safe and appropriate change. Moreover HPV DNA has been shown to be more sensitive in picking up high-grade cervical lesions, which can then be treated to prevent a woman developing cancer.
Dr Annika Antonsson is Senior Research Fellow in the Cancer Control Laboratory at the QIMR Berghofer Medical Research Institute
This paper by Canfell et al investigated the effectiveness of different screening tests for cervical cancer. Almost 100 per cent of all cervical cancers are caused by long-term (over a decade), persistent HPV infections. HPV is very common, especially in younger sexually active adults, and the great majority of people clear HPV infections naturally.
There are more than 200 different types of HPV. All Australian women 33 and younger have been offered free vaccination against potentially cancer causing HPV types 16 and 18, while women older than 33 years have not been offered free HPV vaccination. A high proportion of women aged 33 or younger have received the HPV vaccination. The need for cervical cancer screening in those two age groups of women could be different and it is therefore important to investigate different screening methods.
The current method of screening for cervical cancer is the Pap smear test, which involves checking cervical cells for abnormalities or cell changes that might lead to cervical cancer. Another, newer screening method is to test for HPV directly (the virus that causes the cancer). In this study, HPV tests were done every 5 years and were compared to liquid-based, Pap-smear-type tests done every 2.5 years.
Canfell and colleagues looked at rates of high-grade pre-cancerous changes in the cervical cells. They found that these pre-cancerous cell changes were identified at much higher rates in the groups that were tested for HPV compared to the groups that were tested with Pap smears (regardless of whether they were offered HPV vaccination or not).
Australia will change its cervical cancer screening program on 1 December 2017 from Pap smears to cervical HPV testing and it is therefore important to have a study like this, which shows that the latter detects more cervical pre-cancers.
The HPV vaccine currently in use only protects against 70 per cent of the HPV types that can cause cancer, so it is still very important for all women aged 18-70 to attend cervical cancer screening. The findings of this study emphasise the importance of cervical cancer screening.
Dr Margaret Heffernan is a behavioural researcher on HPV vaccines at RMIT University
This research has been undertaken by internationally recognised and respected Australian cervical cancer and HPV scientists and clinicians. The research methodology is robust and benchmarked against other international studies.
It is piloting the HPV test for quality assurance and safety in a sample that includes women who have received the HPV vaccine. The study found higher detection rates that confirm the viability of introducing the test as a replacement for the current Pap test.
As this is a pilot study the participants are going to be a discrete sample – in this case, women who routinely attend for cervical screening. It would be helpful in a future phase of the Compass study if the trial could be extended to women who do not routinely attend for screening, including women from vulnerable and therefore high-risk populations.
This pilot randomised trial is extremely important in helping health practitioners and agencies make an informed decision about whether to replace population screening for cervical cancer through the current Pap test (the National Cervical Screening Program (NCSP) started in 1991) with HPV testing.
No test is perfect and a weakness with the Pap test is that it cannot detect all high-risk HPV lesions. The Compass study is contributing to findings from other global studies that are proving the reliability of HPV testing over Pap testing on a population basis.
The results of the Compass pilot randomised trial has shown that it is monitoring quality assurance and safety of the HPV test before it is introduced as an alternative screening for cervical cancer. This cautious well-researched approach means that by the time it is offered to women as an alternative it has been rigorously trialled and tested which is important in allaying women’s fears about new procedures.
In the past 25 years there has been much high-quality scientific research undertaken globally on HPV, and particularly since the HPV vaccines were introduced. Therefore we now have a more sophisticated and better understanding of how HPV causes cervical cancer (and other HPV ano-genital cancers) and the time frame that it takes for cervical cancer to develop.
The findings of this research will reassure Australian women that the new changes in screening for cervical cancer that come into effect in late 2017 are a scientific improvement on the Pap test that we currently have, and have better capacity to detect pre-cancer or cancer of the cervix and therefore will help save lives.
The new HPV test is proving to be more precise in detecting changes in cells surrounding the cervix (which if persistent lead to cancer of the cervix). This means that any signs of pre-cancer that the new test detects can be managed medically in a more reliable and quicker time frame.
Therefore, the recommendations that cervical cancer screening via HPV testing be undertaken every five years is based on new knowledge arising from scientific research that has been undertaken around the world, including this Compass trial. This will give women peace of mind. It will also be of great advantage for women who have not had the HPV vaccine, or for those women who find the previous Pap test uncomfortable and embarrassing.
The earlier we have access to this HPV test the better. Prior to the introduction of HPV vaccination Australia had the lowest cervical cancer rates in the world because of our world class Pap screening program. With this new HPV test, combined with the HPV vaccine and good community education we now have the chance to make cervical cancer a thing of the past. Australian women are very lucky that we are being offered HPV testing!



 Australia; NSW; VIC
Australia; NSW; VIC