Media release
From:
Scientists have achieved a major breakthrough by 3D bioprinting miniature placentas, providing a new way to study complications in pregnancy, with research led by the University of Technology Sydney (UTS).
Pregnancy complications lead to over 260,000 maternal deaths and millions of infant deaths globally. One serious condition in pregnancy linked to placental dysfunction is preeclampsia, which affects 5–8% of pregnancies.
The study, led by Associate Professor Lana McClements and first author Dr Claire Richards, from the UTS School of Life Sciences, has just been published in the journal Nature Communications.
“Obtaining first trimester placental tissue is not practical or safe, making early pregnancy challenging to study. By the time a baby is born, the placenta has changed so much that it no longer reflects what it was like in early pregnancy,” said Dr McClements.
“Serious pregnancy complications like preeclampsia remain one of medicine’s great mysteries, largely because current animal and cell models cannot accurately replicate the human placenta,” she said.
Miniature organs, known as ‘organoids’, provided a breakthrough in medical research when they were first described in 2009. Since then, scientists have grown organoids from a wide range of human organs by taking stem cells and setting them in a gel.
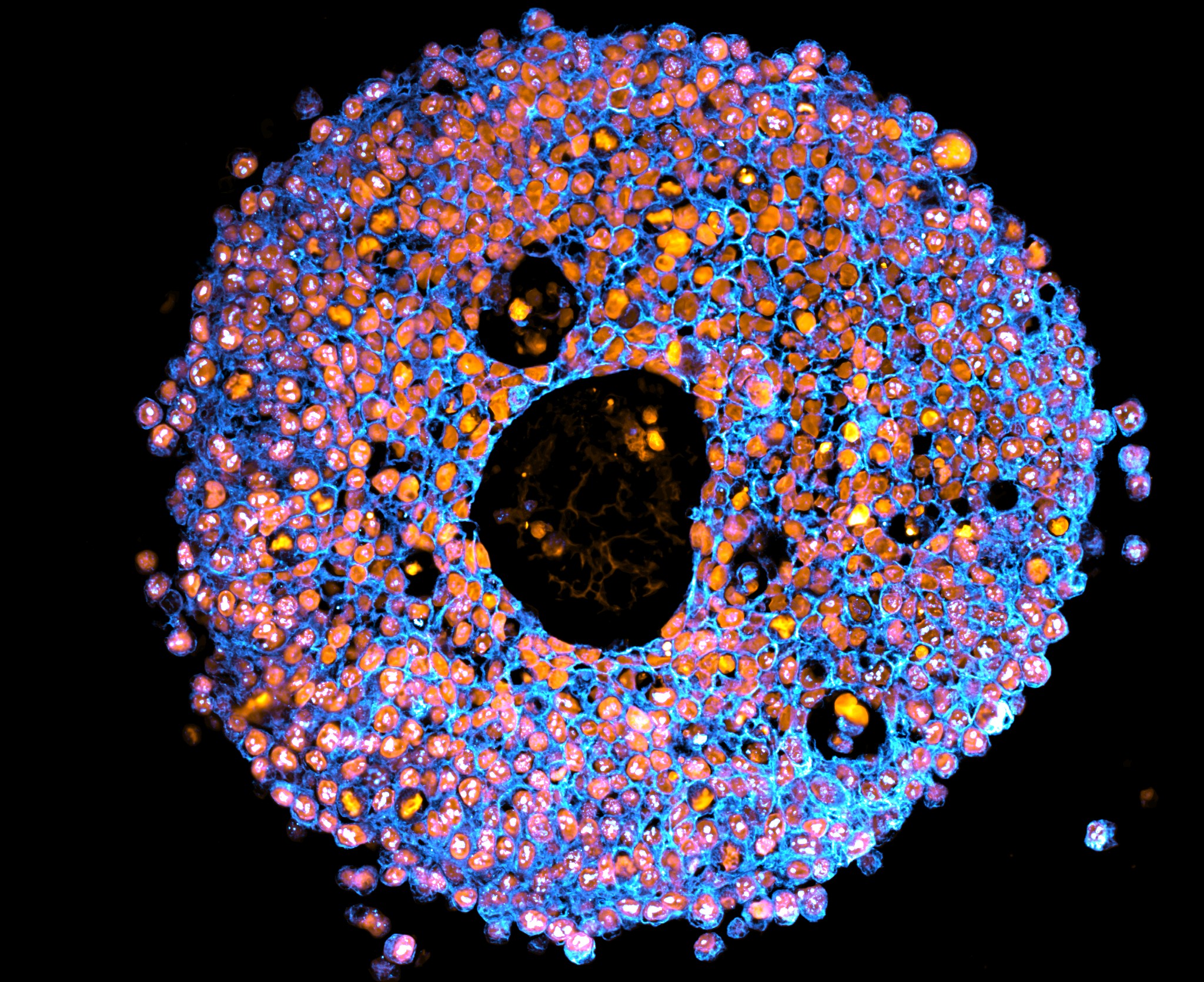
This gel mimics the tissue that cells are supported in and allows them to form clusters as they grow and divide. In 2018, the first placental organoids (or ‘mini placentas’) were grown from trophoblasts – a type of cell found only in the placenta.
Bioprinting is a type of 3D printing technology that uses living cells and cell-friendly materials to create 3D structures. The researchers mixed trophoblast cells with a synthetic, controllable gel and 3D printed them into a culture dish in precise droplets, much like an ink-jet office printer.
“Our printed cells grew into placental organoids and we compared them to organoids made via traditional manual methods,” said Dr Richards.
“The organoids we grew in the bioprinted gel developed differently to those grown in an animal-derived gel, and formed different numbers of trophoblast sub-types. This highlighted that the environment organoids are grown in can control how they mature.
“We showed these organoids were very similar to human placental tissue, providing an accurate model of the early placenta. This means we can start piecing together the puzzle of pregnancy complications and test new drugs safely.
“For example, we exposed our bioprinted organoids to an inflammatory molecule found at high levels in women with preeclampsia, then tested potential treatments to see how the organoids grew and responded.
“As we refine these models, we move closer to a future where pregnancy complications can be predicted, prevented and treated before they put lives at risk.”



 Australia; NSW
Australia; NSW