News release
From:
MAIT Cell Activation May Play a Role in Fatal Outcomes Among Severe COVID-19 Cases
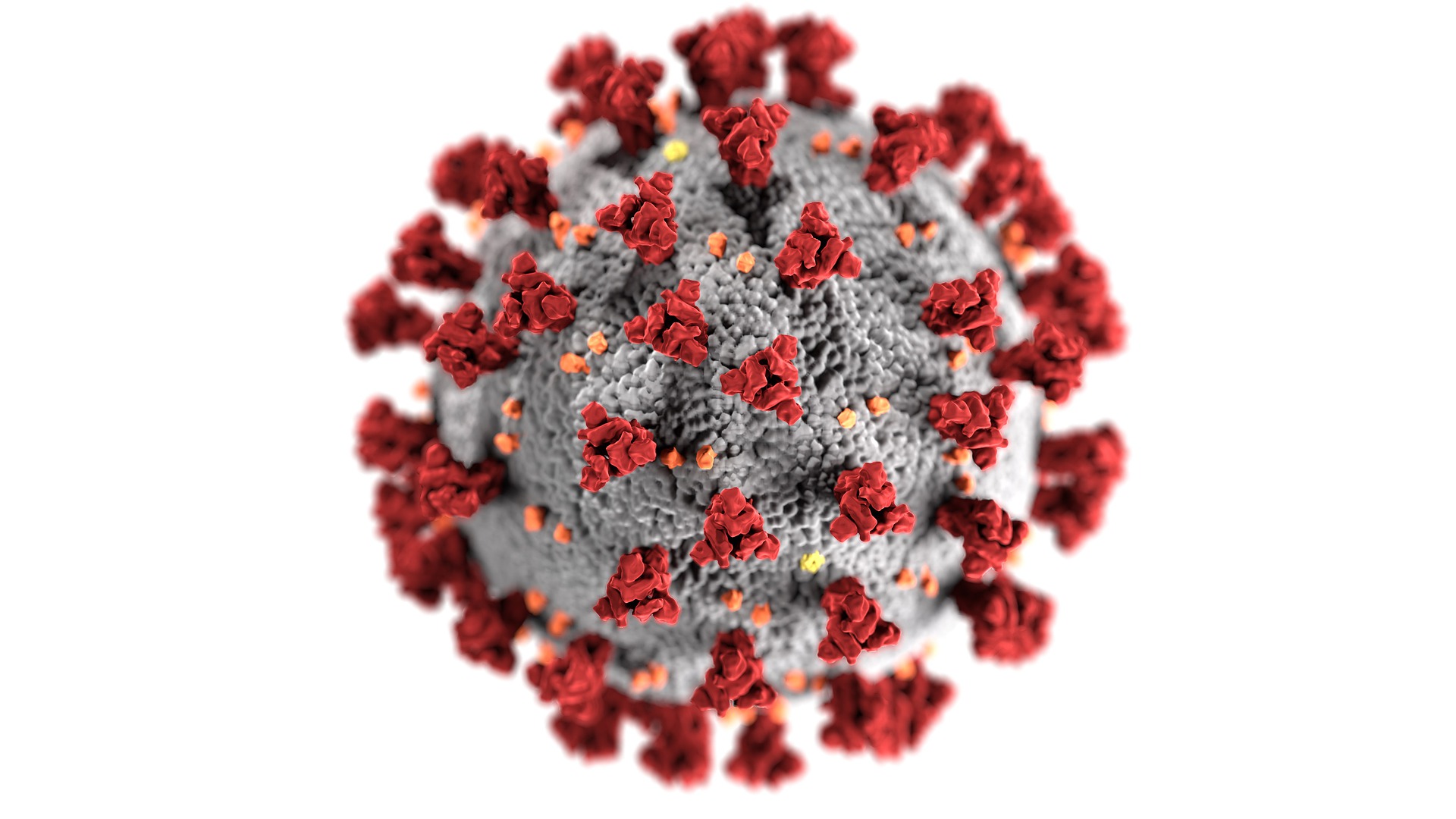
Antibodies and T cells play a critical role in protection from viral illness, however the exact role of T cell and antibody responses in SARS-CoV-2 infection is unclear. To better understand the immune abnormalities linked to critical illness and death in COVID-19 patients on ICU, researchers conducted a prospective observational study investigating the association of T cell and antibody responses with fatal outcome in severe COVID-19. They analyzed serum samples from 41 mechanically ventilated COVID-19 patients, performing immunophenotyping of T cell responses and a range of experiments analyzing antibody responses. They then compared their findings to a parallel set of 18 mechanically ventilated influenza patients, as well as to 12 mild COVID-19 patients and 12 healthy controls.
The researchers found that fatal COVID-19 infections were correlated with poorly coordinated systemic immune responses and elevated mucosal associated invariant (MAIT) cell activation were the strongest predictor of a fatal outcome. However, the study was limited in that it only analyzed samples in a cross sectional manner and did not observe how immune responses changed over the course of the infection. Future studies are needed to explain in depth how mortality-associated immune characteristics may develop over time.
According to the authors, “Our study yields an enhanced understanding of the differential immunopathogenic processes driving critical COVID-19 and influenza, which can translate into improved immunotherapeutic approaches in patients with severe viral pneumonitis.”
“In critically ill patients on ICU with COVID-19 and influenza, an unbiased analysis of the antiviral immune response revealed activation of a specific immune subset -Mucosal-associated invariant T (MAIT) cells - as a strong immunological predictor of death,” the authors add. “Survival in critical COVID-19 is associated with focused immune responses driven mainly by one cytokine - interferon alpha – in contrast to the very broad pro-inflammatory responses seen in those with fatal disease. This cytokine pattern linked to death versus survival separates critical COVID-19 from influenza.”
############



 International
International