News release
From:
Evidence base for using obesity medications to treat adolescents continues to grow, but evidence does not yet exist for use in younger children
*PLEASE MENTION THE INTERNATIONAL CONGRESS ON OBESITY, SAO PAULO, IF USING THIS MATERIAL*
With levels of adult and child obesity continuing to increase in most parts of the world, it is inevitable that all options including medications should be considered to successfully treat obesity in younger people.
In a presentation at this year’s International Congress on Obesity (ICO 2024, Sao Paulo, Brazil, 26-29 June), World Obesity Federation President Professor Louise Baur who is an obesity paediatrician and Professor of Paediatrics at the University of Sydney, NSW, Australia, will discuss the growing evidence base to use obesity medications to treat adolescents, while making clear the evidence is not yet there to use these medications in younger children. Prof Baur will also make clear use of obesity medications among younger people must be in conjunction with continuous lifestyle and diet support.
“Obesity among the youngest in our society is Increasingly common,” explains Professor Baur. “And just as we have realised with adults, obesity is not an acute-care, once-treated-always-cured disease. It is a relapsing and remitting disease also in children and adolescents, and so we must bring a chronic disease care / rehabilitation perspective to the treatment of children and adolescents with obesity.”
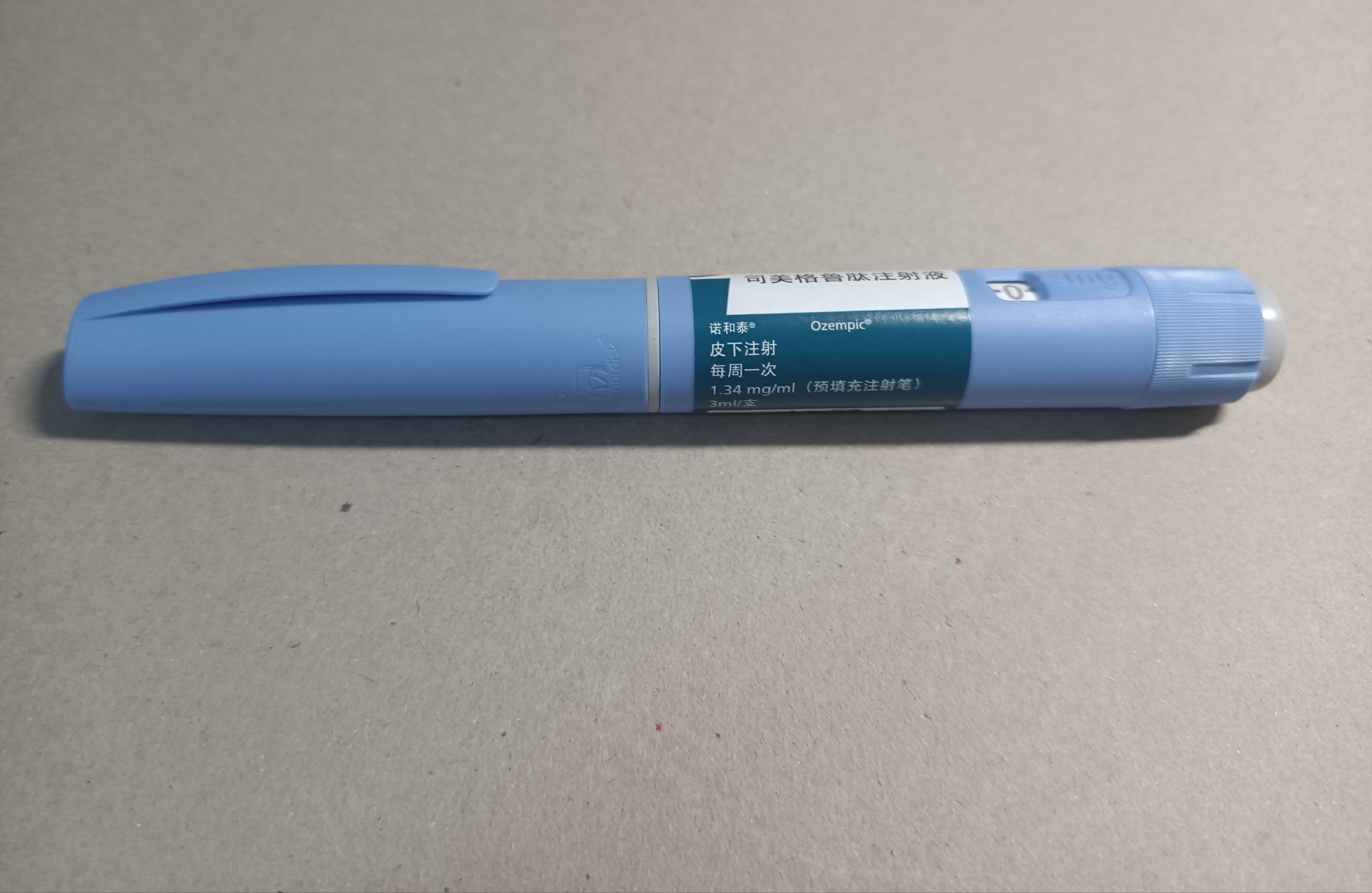
Evidence has also built in recent years about the successful use of obesity (bariatric) surgery to treat obesity in adolescents. Professor Baur says: “The use of the latest generation of obesity management medications could present a less invasive option for adolescents with more severe obesity. The evidence from various recent trials shows that these new medications, such as semaglutide, act in exactly the same way in adolescents as in adults, with a similar safety profile. One of the ways in which semaglutide works is by acting on brain appetite centres, promoting a sense of satiety, reducing hunger and encouraging a decrease in food consumption.”
Professor Baur will discuss the evidence from trials of GLP-1 medications liraglutide and semaglutide, published in NEJM, that led to both being approved to treat obesity by both the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA). She will also discuss the GLP-1/GIP co-agonist tirzepatide, approved for treating obesity in adults and with a trial ongoing to test its efficacy in adolescents.
The other new generation drugs, including GLP1-glucagon co-agonists and tri-agonists (such as retratutide) and GLP-1 amylin co-agonists (CagriSema – a combination of carglinitide and semaglutide) could also have future uses in adolescent obesity treatment, but for now are only being trialled in adults.
Prof Baur concludes: “There is a growing evidence base for some obesity management medications in adolescents – however no evidence exists yet for use in younger children aged under 12 years, but use may be justified in those younger children with more severe obesity.”
She adds: “In all cases, these obesity medications must be used in combination with support for behavioural change, as part of multi-disciplinary, adolescent-friendly care. It is clear from our experience with adults that long-term use will most probably be needed, but further evidence is needed on this.”
“More evidence is also needed for use of these medications in adolescents for maintenance therapy, pretreatment for surgery, post-surgery treatment, combination therapy, and the use of medication with other obesity therapies. Yet as we have found with adults, the cost and availability of these medications are a major barrier in every country.”
This press release is based on the presentation “Current and Future Pharmacotherapies for Obesity in Children and Adolescents” taking place in room 1 from 1400-1530H on Saturday 29 June at the International Congress on Obesity, the Frei Caneca Conventions Center, Sao Paulo.



 Australia; NSW
Australia; NSW