News release
From:
American College of Physicians
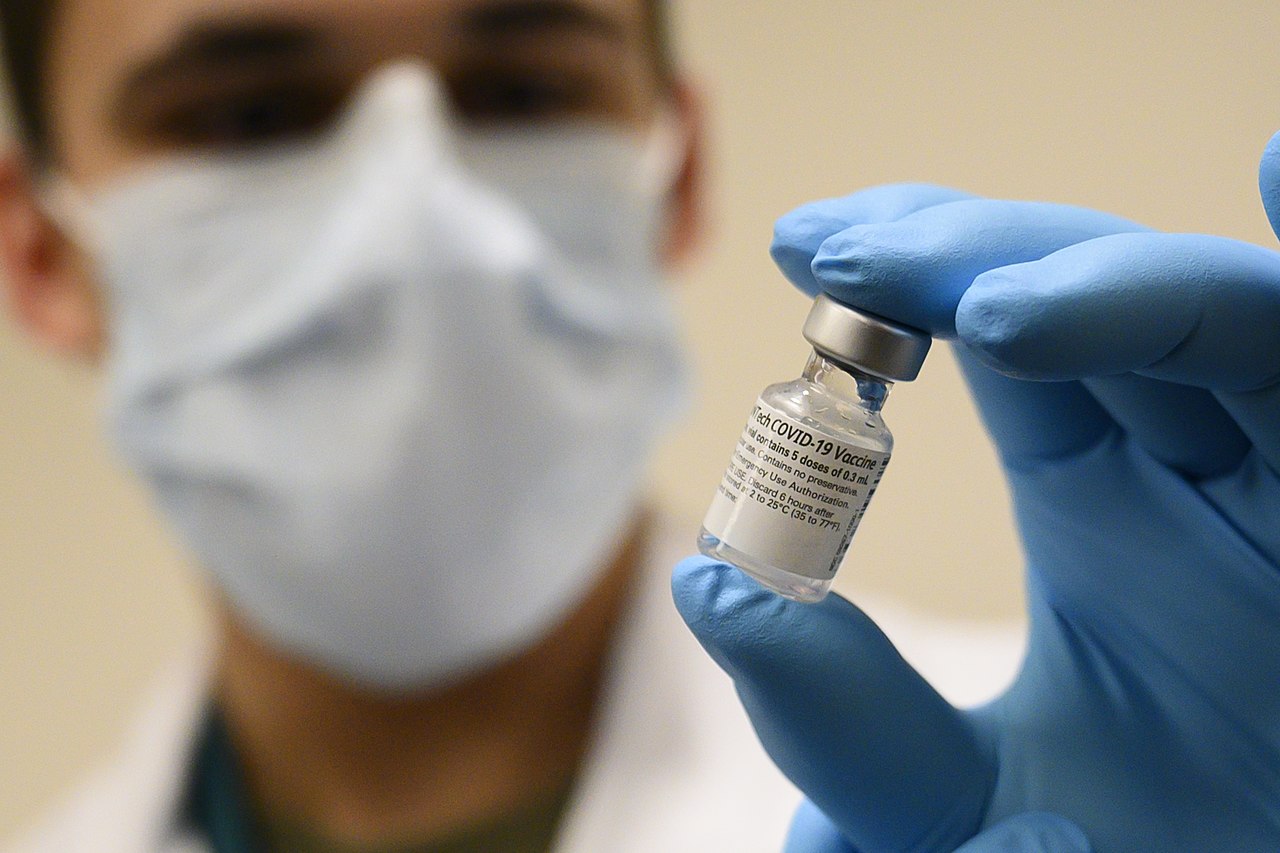
COVID-19 vaccination elicits antibody response in vast majority of immunocompromised patients receiving immunosuppressive therapy
Abstract: https://www.acpjournals.org/doi/10.7326/M21-1757
URL goes live when the embargo lifts
A prospective cohort study found that nearly 90 percent of immunocompromised patients taking glucocorticoids or other immunosuppressive therapy had an antibody response following SARS-CoV-2 vaccination. The response was about a third as strong as that of participants with healthy immune systems but suggests that vaccines could offer some protection to those at risk for severe illness. The findings are published in Annals of Internal Medicine.
Researchers from Washington University School of Medicine in St. Louis and the University of California, San Francisco recruited 133 adults with confirmed chronic inflammatory diseases and 53 immunocompetent volunteers to receive an mRNA vaccine for SARS-CoV-2. Participants provided blood samples within 2 weeks before receiving the first dose of the mRNA vaccine and within 3 weeks after receiving the second dose. The researchers measured each participants’ antibody levels and counted the number of antibody-producing cells in their blood samples. All patients stayed on their prescribed drug regimens, except for three whose medications were paused within one week of immunization.
The researchers found that about 9 out of 10 immunocompetent participants developed antibodies in response to the vaccine, although the response was weaker than for those in the healthy group. Patients taking glucocorticoids and those taking B cell-depleting therapies were at higher risk for not developing an antibody response.
According to the researchers, these findings should encourage immunocompromised patients to get their COVID-19 vaccine. The CDC recently recommended a third dose of vaccine for this patient population, which could elicit an even stronger response.
Journal/
conference:
Annals of Internal Medicine
Organisation/s:
Washington University School of Medicine, USA
Funder:
This research was funded and supported by The Leona M. and Harry B. Helmsley Charitable Trust, the Washington University Digestive Disease Research Core Center (NIDDK P30DK052574), the Washington University Rheumatic Diseases Research Resource-Based Center (NIAMS P30AR073752), The Judy Miniace Research Fund for the Washington University Lupus Clinic, the Washington University Institute of Clinical and Translational Sciences (ICTS) grant UL1TR002345 from the National Center for Advancing Translational Sciences (NCATS), and NIAID Collaborative Influenza Vaccine Innovation Centers contract 75N93019C00051 for the Washington University Infectious Diseases Clinical Research Unit COVID sample collection. The UCSF investigators were funded by a Seeding Bold Ideas Grant from the Marcus Program in Precision Medicine Innovation, PREMIER, a NIAMS P30 Center (P30AR070155), and the Russell/Engleman Rheumatology Research Center. This study utilized samples obtained from the Washington University School of Medicine's COVID-19 biorepository, which is supported by the Barnes-Jewish Hospital Foundation, the Siteman Cancer Center grant P30CA091842 from the National Cancer Institute of the NIH, and the Washington University ICTS grant UL1TR002345 from the NCATS of the NIH. Dr. Deepak is supported by a Junior Faculty Development Award from the American College of Gastroenterology and IBD Plexus of the Crohn's & Colitis Foundation. Dr. Paley is supported by the Rheumatology Research Foundation. Dr. Ciorba is supported by R01DK109384 and by the Lawrence C. Pakula MD IBD Education and Innovation Fund and Pfizer (IIS #61798927). Dr. Wu is supported by the National Institute of Neurological Disorders and Stroke (R01NS106289) and the National Multiple Sclerosis Society (RG-1802-30253). Drs. Nakamura and Gensler are supported by the San Francisco VA Health Care System. Drs. O'Halloran, Presti, and Ellebedy are supported by NIAID Collaborative Influenza Vaccine Innovation Centers contract 75N93019C00051. Dr. Ellebedy is also supported by NIAID grant U01AI141990, NIAID Centers of Excellence for Influenza Research and Surveillance contracts HHSN272201400006C and HHSN272201400008C, and NIAID Collaborative Influenza Vaccine Innovation Centers contract 75N93019C00051. Dr. Alfred Kim is supported by the Rheumatology Research Foundation, NIH/NIAMS P30 AR073752, and PCORI SDM2017C28224.



 International
International