News release
From:
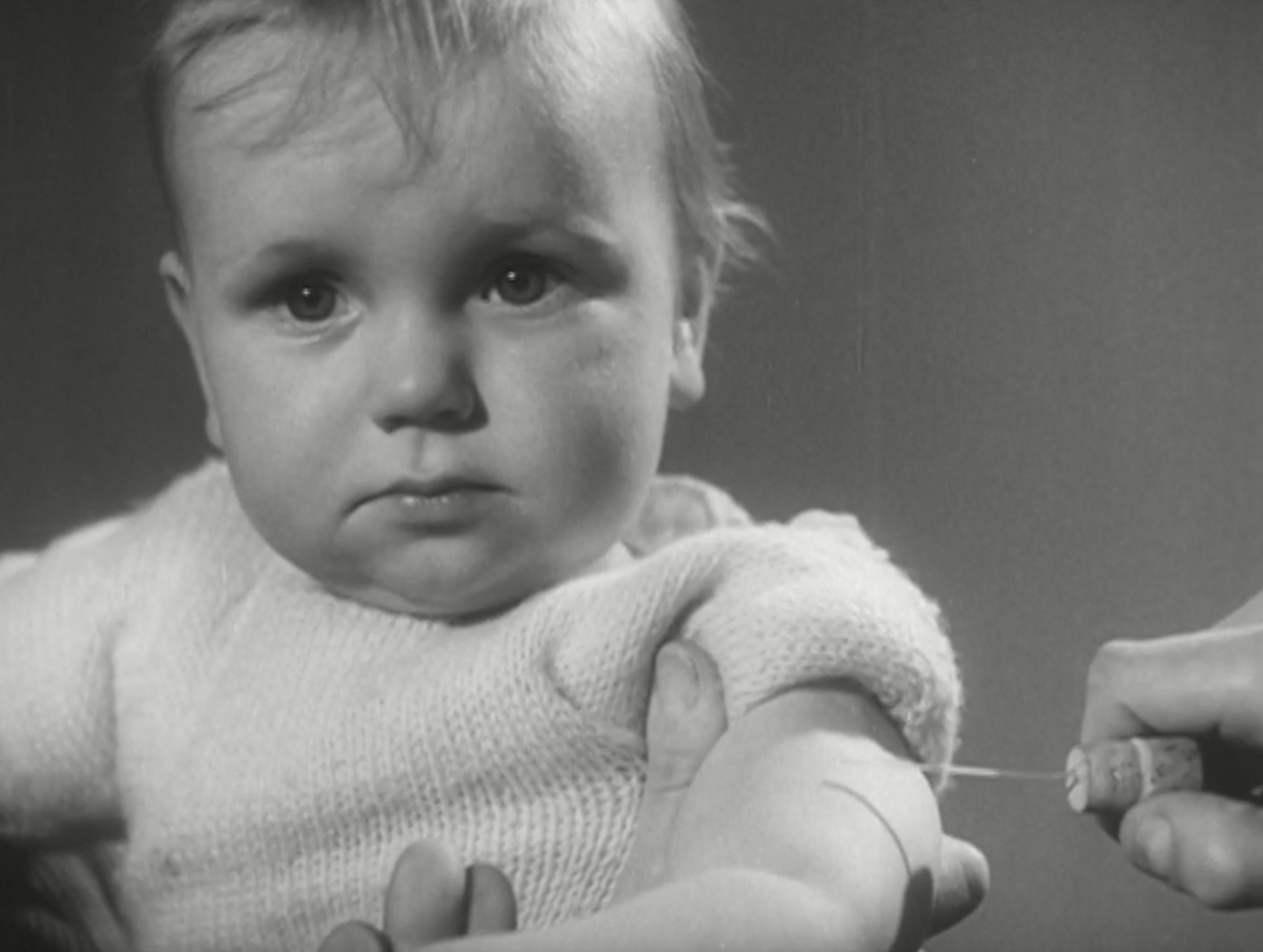
Local infectious disease experience influences vaccine refusal rates: a natural experiment
Summary: Vaccine refusal has increased in recent years and this increase has been linked to complacency associated with reductions in disease risk. We study whether mortality during two smallpox epidemics in Glasgow between 1900 and 1904 mattered for later smallpox vaccine refusal following its legalisation in Scotland in 1907. We find that in small areas of Glasgow where mortality during the epidemics was lower, later vaccine refusal was higher. The finding suggests that complacency also influenced vaccination decisions in a period when infectious disease risk was higher than recently, responding to the local prior experience of the relevant disease.



 International
International