Media release
From: Springer NatureEngland and Wales and Spain experienced the highest numbers of excess deaths as a result of the COVID-19 pandemic from mid-February to May 2020, suggests a modelling study of 19 European countries, and Australia and New Zealand, published in Nature Medicine. The results indicate that around 206,000 additional deaths occurred across these countries than were expected had the pandemic not occurred.
The current COVID-19 pandemic has caused over 1 million deaths directly from SARS-CoV-2 infections globally. However, the indirect effects of the pandemic and responses to it through social, economic, environmental and healthcare pathways can also be substantial. Understanding the total impact of the pandemic on mortality is important for assessing its full impact on public health and policy responses.
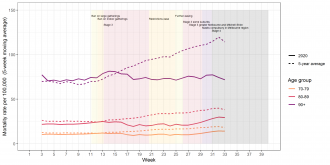
Majid Ezzati and colleagues used weekly data on deaths from 2010 to mid-February 2020, from 21 countries, to create a model that could predict how many deaths would have occurred by May 2020 had there not been a COVID-19 pandemic. They compared this figure with the actual reported deaths in the countries studied to calculate the excess deaths that resulted from the pandemic whether it was from COVID-19 or other causes. The authors estimate that an additional 206,000 deaths had occurred as a result of the pandemic in these 21 countries, with the highest figures for all-cause mortality per 100,000 people in Spain, England and Wales, Italy, Scotland and Belgium. The authors found that the numbers of excess deaths for men and women were similar, with 105,800 deaths in men and 100,000 deaths in women. They indicated that England and Wales and Spain experienced the largest increase in mortality, with nearly 100 excess deaths per 100,000 people, which was an increase of 37% for England and Wales and 38% for Spain, relative to levels without a pandemic.
The authors conclude that the differences in mortality among the 21 countries reflect the variability in characteristics of the populations, policy responses to the pandemic, the preparedness of public health systems, and extent of community-based and facility-based care systems. They argue that in addition to suppressing transmission, building integrated care pathways to allow appropriate triage and care for those with long-term health conditions will be important for minimizing deaths resulting both directly and indirectly from the ongoing pandemic. To achieve this, countries may need to reallocate and expand healthcare resources, particularly in settings in which there has been underinvestment in health and social care systems, they suggest.



Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Dr Paul Read is Senior Research Fellow at the Monash Sustainability Institute at Monash University. His multidisciplinary work combines human nature, crime, health and sustainability.
Adjunct Professor Brett Sutton is Chief Health Officer in the Victorian Department of Health and Human Services