EXPERT Q&A: The Mu variant and future of 'endemic' COVID-19
Not peer-reviewed: This work has not been scrutinised by independent experts, or the story does not contain research data to review (for example an opinion piece). If you are reporting on research that has yet to go through peer-review (eg. conference abstracts and preprints) be aware that the findings can change during the peer review process.
Opinion piece/editorial: This work is based on the opinions of the author(s)/institution.
Opinion piece/editorial: This work is based on the opinions of the author(s)/institution.
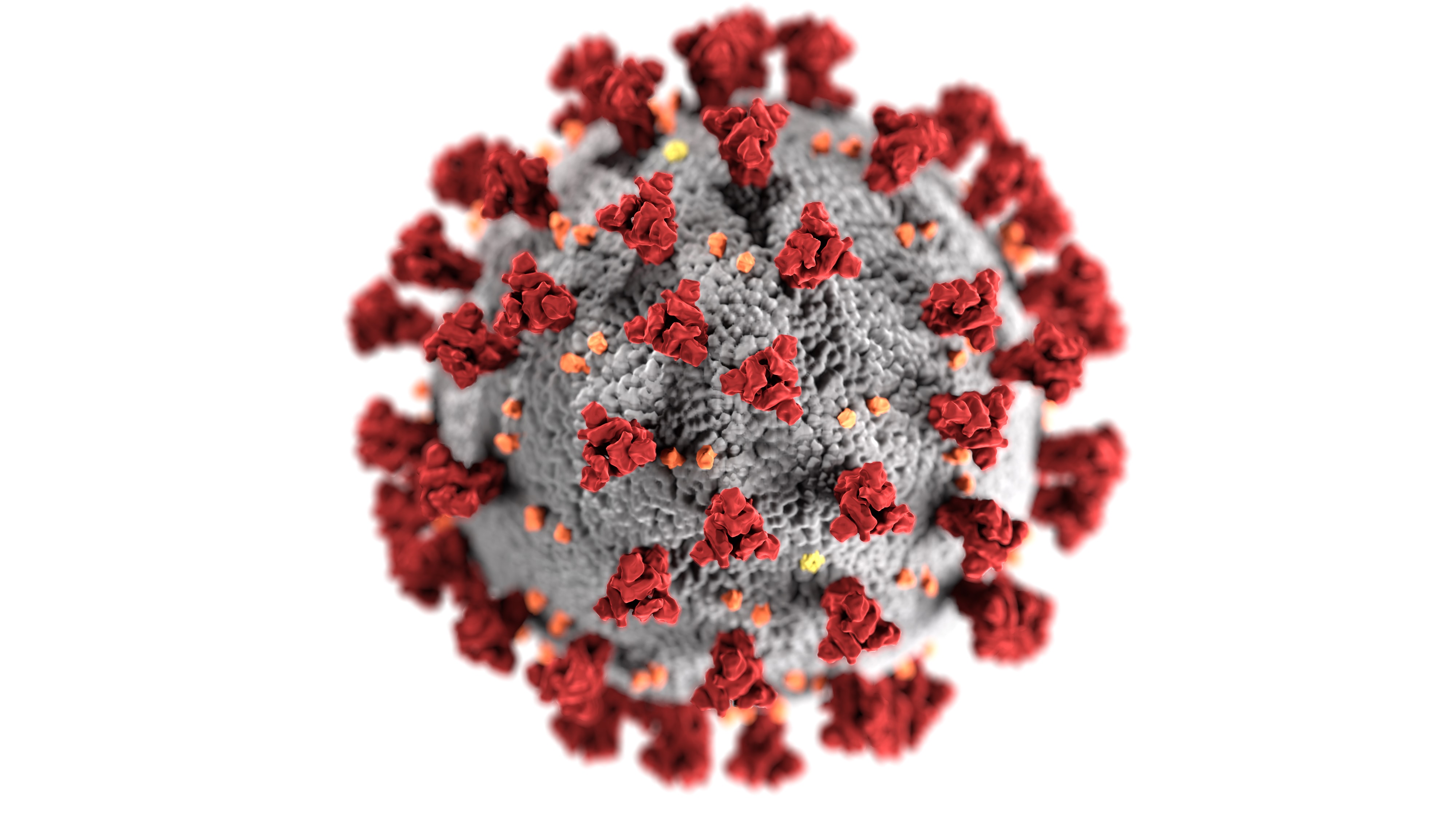
The world has a new COVID-19 variant of interest, with the WHO recently reclassifying the Mu variant after an uptick in cases in South America. With fears this variant could be better at evading vaccines, concerns grow over the possibility of new variants making COVID-19 endemic, or consistently present in society. Dr Vinod Balasubramaniam, a virologist from Monash University Malaysia, answers questions about what Mu and variants yet to arise could mean for the future of COVID-19.
Organisation/s: Monash University
Funder: N/A
News for:
Australia
International
VIC
Media contact details for this story are only visible to registered journalists.


Expert Reaction
These comments have been collated by the Science Media Centre to provide a variety of expert perspectives on this issue. Feel free to use these quotes in your stories. Views expressed are the personal opinions of the experts named. They do not represent the views of the SMC or any other organisation unless specifically stated.
Dr Vinod Balasubramaniam is a virologist at the Jeffrey Cheah School of Medicine & Health Sciences at Monash University Malaysia